When your shoulder starts to hurt and won’t move-no matter how hard you try-it’s easy to think it’s just a bad strain or a pinched nerve. But if the pain creeps in slowly, gets worse at night, and your arm feels locked in place even when someone else tries to move it, you might be dealing with something more specific: frozen shoulder, or adhesive capsulitis.
This isn’t just stiffness. It’s your shoulder joint capsule-the bag of tissue that holds everything together-thickening, tightening, and shrinking. Studies show the capsule can lose nearly half its volume, dropping from a normal 30-35 mL down to just 10-15 mL. That’s like trying to stretch a shrunken T-shirt over your shoulder. The result? Pain that doesn’t go away, and movement that feels impossible.
What Happens Inside Your Shoulder?
The shoulder joint is the most mobile in your body, but that flexibility comes at a cost: it’s unstable. The joint capsule wraps around the ball-and-socket joint, lined with a thin layer of tissue called the synovium. In frozen shoulder, that lining becomes inflamed. Over time, it turns into scar tissue. This isn’t glue sticking things together, despite the name “adhesive” capsulitis. It’s a contracture-a tightening that pulls the capsule down like a drawstring.
The tightness follows a clear pattern. External rotation (turning your palm up) is hit hardest-often 60-70% lost. Then comes abduction (lifting your arm out to the side), followed by internal rotation (reaching behind your back). If you can’t scratch your back or reach into your back pocket, this is why. And it’s not just you moving the arm-your doctor or therapist can’t move it much either. That’s the key difference from a rotator cuff tear, where passive motion (someone else moving your arm) is still possible.
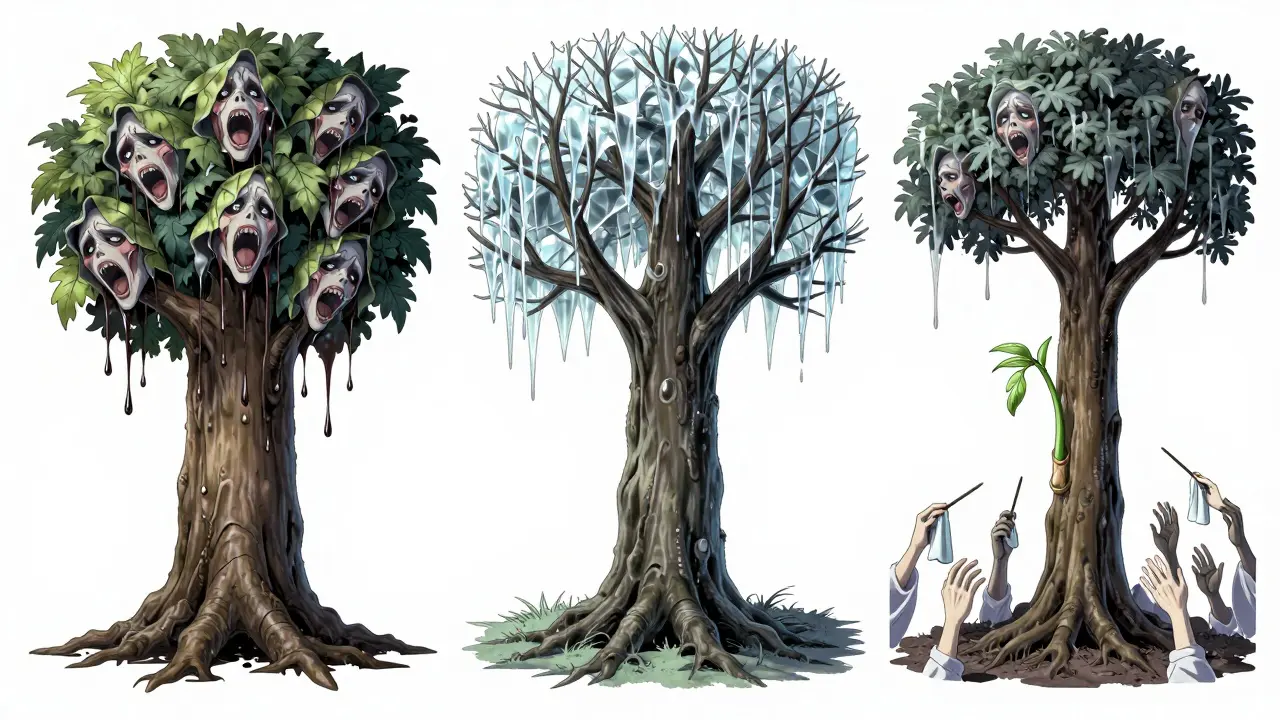
The Three Stages of Frozen Shoulder
This condition doesn’t hit all at once. It unfolds in three stages, and knowing which one you’re in changes everything about how you treat it.
Stage 1: Freezing (6 weeks to 9 months)
Pain is the main player here. It starts mild, then builds. You might notice it more at night-waking up because your shoulder feels like it’s on fire. Movement hurts, but you can still move it, even if it’s painful. This is the most confusing stage. Many people think rest will help. It won’t. In fact, doing nothing makes it worse.
Stage 2: Frozen (4 to 6 months)
Pain starts to fade, but stiffness takes over. This is when people say, “It doesn’t hurt as much, but I can’t move it at all.” You might still be able to lift your arm a little, but not beyond shoulder height. Reaching behind your head or putting on a seatbelt becomes impossible. This is the stage where most people finally seek help-because they can’t live like this.
Stage 3: Thawing (6 months to 2 years)
Slowly, movement returns. Not fast, not dramatically, but it comes. You start getting back a few degrees of motion each week. This stage can last a long time without treatment. With the right mobilization, it can shrink from two years to under six months.
Who Gets Frozen Shoulder-and Why?
It’s not just something that happens to older people. While it’s most common between ages 40 and 60, anyone can get it. But certain groups are at much higher risk.
People with diabetes are 10 to 20 times more likely to develop frozen shoulder. Why? High blood sugar causes abnormal collagen buildup in tissues-including the shoulder capsule. Thyroid disorders, heart disease, and Parkinson’s also increase risk. Even if you’re otherwise healthy, a shoulder injury, surgery, or long period of immobilization (like after a broken arm) can trigger it.
And here’s the catch: it’s misdiagnosed nearly half the time. Many doctors mistake it for a rotator cuff tear or arthritis. The clue? If both active and passive motion are limited equally, and you have no history of trauma, it’s likely frozen shoulder.

Mobilization Strategies That Actually Work
Here’s the good news: frozen shoulder almost always gets better. But waiting it out isn’t the best plan. Studies show that with the right mobilization, recovery time drops from 24-40 months to 6-12 months.
The key? Timing and technique. What works in the freezing stage can hurt you in the frozen stage.
During the Freezing Stage: Gentle Motion Only
Forcing your shoulder to move beyond pain causes more inflammation. Think of it like poking a bruise. You don’t want to make it worse.
- Pendulum exercises: Lean forward, let your arm hang loose. Gently swing it in small circles-clockwise and counterclockwise-for 5 minutes, twice a day. This keeps the joint lubricated without stressing it.
- Towel stretch: Hold a towel behind your back with both hands. Use your good arm to gently pull the towel upward, helping the affected arm stretch. Don’t force it-just enough to feel a mild pull.
- Heat before movement: Apply a warm towel or heating pad for 10 minutes before exercises. Heat relaxes the capsule and makes stretching safer.
Research from Healthgrades shows patients who started these moves within 8 weeks of symptoms had 65% less pain at 6 months compared to those who waited.
During the Frozen Stage: Gradual Progression
Pain is lower, so you can do more. But you still need patience. This is where supervised physical therapy makes the biggest difference.
- Doorway stretch: Stand in a doorway, place your hand on the frame at shoulder height. Gently lean forward until you feel a stretch across the front of your shoulder. Hold 30 seconds. Repeat 3 times.
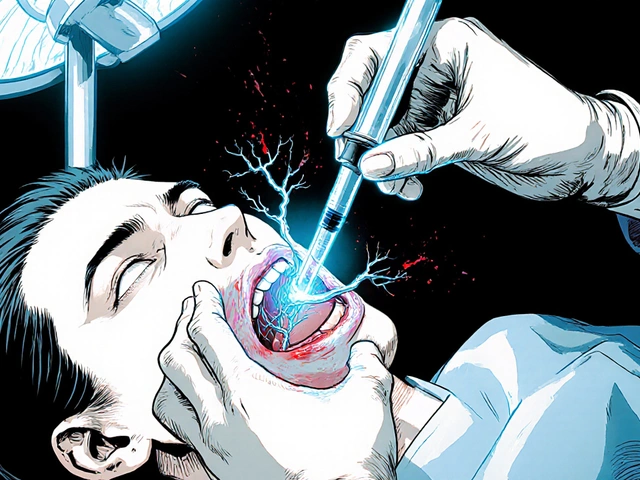
- Wand exercises: Use a broomstick or a special rehab wand. Lie on your back, hold the wand with both hands. Use your good arm to lift the affected arm overhead, slowly. Stop at the point of resistance-not pain.
- External rotation stretch: Lie on your side with the affected shoulder down. Bend your elbow to 90 degrees. Use your good hand to gently push your forearm toward the floor, increasing external rotation.
Patients in a 2023 study using a device called ShoulderROM (which tracks motion in real time) recovered 32% faster than those doing standard exercises. The feedback helped them stay within safe limits.
What Doesn’t Work (and Can Make Things Worse)
Not all advice is good advice.
Aggressive stretching during the freezing stage? That’s a common mistake. One patient on Cleveland Clinic’s review said forced cross-body stretches turned their pain from 4/10 to 8/10 for three weeks. That’s not progress-that’s injury.
Manipulation under anesthesia (MUA)-where a doctor forcibly moves your shoulder while you’re asleep-is sometimes offered. But it’s risky. The AAOS says it should only be considered after 6 months of failed conservative care. It can cause fractures, nerve damage, or torn tendons if done too early.
Corticosteroid injections? They help some people with short-term pain relief (4-8 weeks), but studies show no real improvement in long-term mobility. They’re not a cure.
What You Can Do Today
You don’t need expensive gear. A towel, a doorframe, and a heating pad are enough to start.
Here’s your daily plan:
- Morning: Apply heat to your shoulder for 10 minutes.
- After heat: Do 5 minutes of pendulum swings.
- Afternoon: Do 3 sets of towel stretch (30 seconds each).
- Evening: Do 3 sets of doorway stretch (30 seconds each).
Track your progress. Measure how far you can reach overhead or behind your back every week. Even 5 degrees of improvement is a win.
Most people see results in 4-6 weeks. If you’re not moving better by then, or if pain spikes, see a physical therapist. Don’t wait until you can’t button your shirt.
Support and Real-World Help
You’re not alone. Over 12,000 people are in the Adhesive Capsulitis Support Group on Facebook. They share videos of their exercises, tips for sleeping better, and stories of recovery.
Many employers now cover virtual physical therapy for conditions like this. If you’re working remotely or have a corporate health plan, check if you have access to telehealth rehab.
And if you have diabetes? Managing your blood sugar isn’t just about your heart or kidneys-it’s directly linked to how fast your shoulder heals.
When to See a Doctor
Most cases resolve on their own. But some red flags mean something else is going on:
- Fever or night sweats
- Unexplained weight loss
- Swelling or redness in the shoulder
- Pain that spreads down your arm or into your neck
If you have any of these, get checked. It could be an infection, tumor, or nerve issue.
For most people, though, frozen shoulder is just a long, slow road back to movement. And with the right approach, it doesn’t have to take years.
Can frozen shoulder go away on its own without treatment?
Yes, frozen shoulder can resolve on its own, but it often takes 1 to 3 years. Without treatment, most people regain full motion, but many are left with lingering stiffness or discomfort. Early mobilization can cut recovery time in half-down to 6 to 12 months.
Is frozen shoulder the same as a rotator cuff tear?
No. A rotator cuff tear involves damage to the tendons that stabilize the shoulder. With a tear, you can usually still move your shoulder passively (someone else can move it for you), and pain is often sharp and localized. With frozen shoulder, both active and passive motion are severely limited, and the pain is dull and constant, especially at night.
Why does my frozen shoulder hurt more at night?
At night, your body is still, and inflammation builds up in the joint. Also, lying on the affected side puts pressure on the capsule, and without distractions, you notice the pain more. Sleeping on your back with a pillow under the affected arm can help reduce pressure and improve comfort.
Should I use ice or heat for frozen shoulder pain?
Use heat before stretching or exercising to relax the tight capsule. Use ice only if you have a flare-up after activity-apply it for 15 minutes to reduce swelling. Heat helps mobility; ice helps inflammation from overdoing it.
Can I do these exercises at home, or do I need a therapist?
You can start with simple exercises at home, especially in the early stages. But if you’re not improving after 4-6 weeks, or if you’re unsure about proper form, seeing a physical therapist is critical. Studies show supervised therapy leads to 28% faster recovery than home-only programs.
Is surgery ever needed for frozen shoulder?
Surgery is rare-only about 13% of cases require it. It’s usually considered only after 6 to 12 months of consistent physical therapy with no progress. Procedures like arthroscopic capsular release can remove scar tissue and restore motion, but they’re not a first-line option.
Does diabetes make frozen shoulder worse?
Yes. People with diabetes are 10 to 20 times more likely to develop frozen shoulder, and their recovery tends to be slower. High blood sugar causes excess collagen buildup in tissues, making the joint capsule stiffer and harder to stretch. Controlling blood sugar levels can improve outcomes.
How long should I do each exercise?
Start with 5 minutes total per session-split between pendulums, towel stretches, and doorway stretches. Do them twice a day. As you improve, increase to 10-15 minutes. Consistency matters more than duration. Five minutes daily is better than 30 minutes once a week.





12 Comments
amanda s
December 17, 2025 AT 19:10 PMThis is the most overhyped medical condition I've ever seen. Everyone's got a frozen shoulder these days. I bet half these people just don't want to go to the gym anymore and are looking for an excuse. I had a rotator cuff tear and I didn't whine about it for two years. Just move your damn arm.
Jigar shah
December 18, 2025 AT 15:42 PMThank you for this comprehensive breakdown. The distinction between passive and active motion limitation is clinically crucial and often misunderstood. I appreciate the emphasis on staging-many clinicians rush into aggressive therapy during the freezing phase, which can exacerbate inflammation. The data on collagen deposition in diabetics is particularly compelling and warrants broader patient education.
Nishant Desae
December 18, 2025 AT 21:34 PMHey everyone, I just wanted to say I’ve been through this twice-once after my shoulder surgery and again when I got diabetic neuropathy. It’s brutal, no lie. But the pendulum exercises? Game changer. I didn’t believe it at first, but doing them every morning before coffee, even when I felt like crying, made all the difference. My wife started doing them with me, and now we do it together. It’s not just about the shoulder-it’s about showing up for yourself, even on the days you want to quit. You’re not alone in this. I’m rooting for you. Keep going. One degree at a time. You got this.
Meghan O'Shaughnessy
December 19, 2025 AT 11:28 AMAs someone who moved from the US to Germany and then back, I’ve seen how differently physical therapy is approached in each country. In the US, it’s all about quick fixes and insurance limits. In Europe, they take the long view-30-minute sessions, weekly check-ins, patience. This article nails the patience part. Also, sleeping on your back with a pillow under the arm? Genius. I wish I’d known that two years ago.
Jody Patrick
December 19, 2025 AT 14:01 PMSimple tip: Use a warm water bottle instead of a heating pad. Cheaper, safer, and you can hug it while you do the stretches. Also, if you’re diabetic, check your sugar before and after exercise. High sugar = more pain. Low sugar = dizzy. Balance is key.
Radhika M
December 20, 2025 AT 07:35 AMMy mom had this for 18 months. She did everything right-heat, towels, gentle swings-but still suffered. Then she tried acupuncture. Not magic, but it helped the pain enough to keep doing the exercises. Worth a shot if you’re stuck.
Philippa Skiadopoulou
December 21, 2025 AT 17:39 PMWhile the mobilization strategies are sound, the omission of evidence-based manual therapy techniques by qualified physiotherapists is notable. Passive mobilization graded to tissue resistance, particularly in the frozen phase, demonstrates superior outcomes in randomized trials compared to home exercises alone. Professional guidance remains indispensable.
Pawan Chaudhary
December 22, 2025 AT 17:43 PMJust wanted to say I’m 3 months in and my shoulder finally started moving again! I was ready to give up, but kept doing the towel stretch every night before bed. Now I can reach my back pocket. Small win, but it means everything. You’re all doing amazing. Keep going!
Jonathan Morris
December 24, 2025 AT 12:52 PMLet’s be real-this is all Big Pharma’s way of selling you physical therapy packages and ShoulderROM devices. The real cause? 5G radiation weakening connective tissue. And why do diabetics get it more? Because they’re being monitored more closely. Coincidence? I think not. The government doesn’t want you to know you can heal with lemon water and fasting. Read the studies. They’re funded by orthopedic corporations.
Linda Caldwell
December 26, 2025 AT 00:27 AMI was told it would take two years. I did it in five months. Not because I’m special-because I showed up. Every single day. Even when I hated it. Even when I cried. Even when my dog looked at me like I was crazy doing pendulums in the kitchen at 6am. Progress isn’t loud. It’s quiet. It’s consistency. You don’t need a fancy device. You need to show up. And you’re already doing that by reading this. That’s half the battle.
Anna Giakoumakatou
December 26, 2025 AT 05:11 AMHow poetic that our most mobile joint becomes our most imprisoned. We live in a world that worships speed, yet the shoulder-this ancient, beautiful, overworked wonder-demands slowness. To move again, we must first surrender to stillness. The capsule doesn’t heal because we force it. It heals because we listen. And isn’t that the real lesson? Not the towel stretch. Not the heat. But the humility to wait. To breathe. To be patient with the body that carries us through every storm.
CAROL MUTISO
December 27, 2025 AT 14:28 PMLook, I get it. You want to fix it fast. But this isn’t a bug to be patched-it’s a conversation your body is having with you. And if you’re ignoring it because you’re too busy scrolling or hustling or pretending you’re fine, then yeah, it’s gonna scream louder. I’ve seen people come back from this with more mobility than before. Not because they pushed harder. Because they finally stopped fighting themselves. That’s the real therapy. The rest? Just the soundtrack.