When your knee hurts just to stand up, you’re not alone
More than knee osteoarthritis pain affects 250 million people worldwide. It’s not just aging - it’s wear and tear on the joint, inflammation, and muscles that have forgotten how to support you. The good news? You don’t need surgery to feel better. Three proven, non-surgical options - bracing, injections, and exercise - can cut your pain by half or more. But not all of them work the same way. And mixing them up wrong can make things worse.
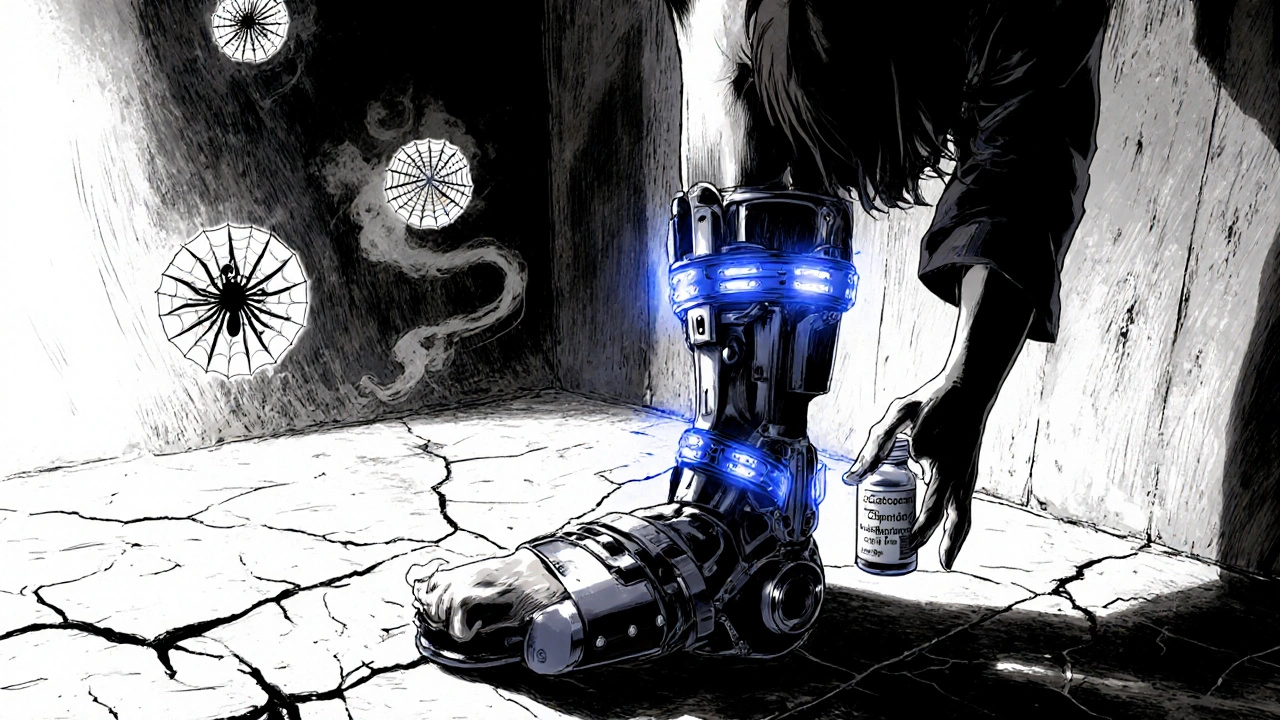
Bracing: The Silent Hero That Shifts Pressure Away From Your Pain
Think of a knee brace like a subtle hand pushing your joint into a better position. Unloader braces, designed for medial compartment OA (the most common type), gently pull weight off the damaged side of your knee. In a 2023 review of 139 studies, patients using these braces saw a 30-45% drop in pain scores. That’s not a small win - it’s the difference between needing help to get out of a chair and doing it on your own.
They’re not magic. You need the right fit. A poorly fitted brace rubs, slips, or does nothing. That’s why seeing a certified orthotist matters. Insurance might cover part of it - Medicare pays 80% of FDA-approved braces - but you’ll still pay the deductible. Prices range from $300 to $1,200. Most people adjust in 2-3 weeks. Once you get used to it, you’ll notice pain drops during walking, climbing stairs, or standing for long periods.
Real talk: 82% of 5-star Amazon reviews mention immediate relief while walking. But 47% of 1-star reviews complain about skin irritation or bulkiness. If you’re active, look for lightweight models with breathable fabric. Some newer ones, like Össur’s Unloader One Pulse, even have sensors that track your gait and give feedback through an app.
Injections: Fast Relief, But Not a Long-Term Fix
If you need quick pain relief - say, before a family event or to get back on your feet after a flare-up - injections are the fastest option. But they’re not meant to be your main strategy.
Corticosteroid shots are the most common. They cost $50-$150 per injection and usually work within days. Studies show they cut pain for 4-12 weeks. But get too many - more than 3-4 a year - and you risk damaging cartilage. The FDA warns against repeated use. Patients on Healthgrades gave them 3.8 out of 5 stars. Why? 32% reported “rebound pain” after the relief wore off.
Hyaluronic acid injections (like Gel-Syn 3, newly FDA-approved in 2023) act like synthetic joint fluid. They cost $500-$1,200 per shot, often requiring 3-5 weekly injections. They last longer - up to 22 weeks in newer formulations - but studies show they’re only slightly better than placebo for most people. And they’re not always covered by insurance.
PRP (platelet-rich plasma) and botulinum toxin are newer options. PRP costs $500-$2,000 per injection and uses your own blood to trigger healing. Evidence is mixed. Botulinum toxin, used off-label, relaxes muscles around the knee to reduce pressure. It’s promising but still experimental.
The catch? Injections have a 0.1-0.7% risk of infection per series. And if you rely on them without moving your joint, your muscles weaken. Dr. Scott Rodeo from Hospital for Special Surgery says overusing injections without exercise can actually speed up decline.

Exercise: The Only Treatment That Gets Better With Time
This is where most people give up - and where the real power lies.
Exercise doesn’t just reduce pain. It rebuilds the muscles that support your knee. In a 12-week study, water-based exercise reduced pain by 28.7% on the Visual Analog Scale. Land-based exercise? 22.3%. Both require 2-3 sessions a week, 45-60 minutes each. The key? Consistency.
Range of motion improves too. After 6-8 weeks of daily stretching, people gained an average of 8.2 degrees in total knee movement. That’s enough to bend deeper, stand up easier, and walk without limping.
But here’s the hard truth: 25-35% of people quit exercise within a year. Why? It’s hard. It’s slow. You don’t feel it the next day. Unlike a shot that numbs pain instantly, exercise makes you sore first, then strong later.
That’s why starting with a physical therapist is critical. Learn the right form for quad sets, heel slides, straight leg raises, and step-ups. Do them wrong, and you hurt more. Do them right, and you’ll notice your hip and ankle pain also drop. That’s because your whole body moves better.
Patients on Healthgrades gave exercise therapy 4.2 out of 5 stars. Why? 78% said they felt significantly better after 12 weeks. And 63% said they noticed less pain in other joints - because stronger knees mean better posture and movement overall.
What Works Best Together - And What Doesn’t
Doctors used to treat these options separately. Now, the best results come from combining them.
Dr. Tuhina Neogi, a leading rheumatologist, says: “Exercise plus bracing plus occasional injections for flare-ups is the most comprehensive approach.”
Here’s how it works in real life:
- Brace during daily activity to reduce joint stress.
- Exercise 3 times a week to rebuild strength and flexibility.
- Injections only when pain spikes - no more than 3-4 times a year.
Studies show this combo beats any single treatment. Bracing improves function scores (SUCRA 92.1%), exercise gives the best long-term results (32.5% improvement at 12 months), and injections give fast relief when you need it.
Don’t do this: Use injections as your only tool. Skip exercise because “the shot fixed it.” That’s like putting a bandage on a broken leg and calling it healed. Your muscles atrophy. Your joint stiffens. Pain comes back worse.

What to Expect - And When to Quit
Bracing: You’ll feel better in days. But give it 2-3 weeks to adjust. If it causes open sores, numbness, or doesn’t reduce pain after 4 weeks, get it refitted or try a different style.
Injections: Pain relief should start within 2-7 days. If you still hurt after 2 weeks, it didn’t work. If you get an infection (redness, swelling, fever), go to the ER immediately.
Exercise: Don’t expect miracles in a week. It takes 12-16 weeks to see real gains. If you’re in more pain after 2 weeks of proper form, stop and see a PT. You might need a different program.
Adherence is everything. In a study of 1,284 patients, 89% stuck with bracing after a year. 92% kept up with injections. Only 48% kept exercising. That’s not because exercise doesn’t work. It’s because it demands more from you.
What’s Changing Right Now
The field is shifting fast. In 2023, the FDA approved a new hyaluronic acid formula that lasts 22 weeks. Smart braces with sensors are now available. And health systems are starting to bundle all three treatments into one care plan.
Insurance coverage is still messy. Medicare covers 80% of braces and corticosteroids, but often denies hyaluronic acid unless you’ve tried everything else. PRP is rarely covered.
The future? Personalized treatment. Researchers are testing if your gait pattern, genetics, or joint structure can predict which treatment will work best for you. Within five years, your orthopedist might give you a prescription for a custom exercise program - synced to a smart brace - based on your unique biomechanics.
Bottom Line: What to Do Today
If your knee hurts daily:
- Get fitted for an unloader brace by a certified orthotist. Don’t buy one online without trying it on.
- Start a supervised exercise program. Look for physical therapy clinics that specialize in OA. Do it 3 times a week.
- Only consider injections if pain flares up badly. Use them as a reset button, not a crutch.
- Track your progress. Use a simple pain scale: 1 = no pain, 10 = unbearable. Recheck every 4 weeks.
Knee osteoarthritis pain doesn’t have to control your life. Surgery isn’t the only answer. The tools are here. You just need to use them the right way - together, consistently, and without shortcuts.
Can I use a knee brace and do exercise at the same time?
Yes - and you should. Braces reduce joint stress during movement, while exercise rebuilds the muscles that stabilize your knee. Many patients wear their brace during daily activities and do their exercise routine without it. This combination gives you immediate support and long-term strength. Just make sure the brace doesn’t restrict your range of motion during exercises like heel slides or quad sets.
How often should I get knee injections?
Corticosteroid injections should be limited to 3-4 times per year. More than that increases the risk of cartilage damage. Hyaluronic acid injections are often given as a series of 3-5 shots over a few weeks, then repeated only if pain returns after 6-12 months. PRP and botulinum toxin have no official guidelines yet, but most doctors recommend no more than 2 treatments per year. Always space injections at least 3 months apart.
What’s the best exercise for knee osteoarthritis?
The most effective exercises are low-impact and focus on strength and mobility. Start with: straight leg raises, seated knee extensions, heel slides, wall squats (only to 45 degrees), and water walking. Avoid high-impact moves like running, jumping, or deep lunges. Water-based exercise is especially good - it reduces joint load by up to 80%. The Arthritis Foundation’s exercise program is a reliable, free resource to follow.
Do knee injections hurt?
Yes - briefly. The needle goes into the joint, which can feel like a sharp pinch. Most doctors use a local anesthetic to numb the skin, but you’ll still feel pressure. Afterward, you might have mild soreness for 1-2 days. Some patients report a “flare-up” of pain 24-48 hours after the shot - this is normal and usually fades. If pain worsens after 3 days, contact your doctor.
Will losing weight help my knee pain?
Absolutely. Every pound lost reduces 4 pounds of pressure on your knee. Losing just 10 pounds can cut your pain by 50% in some cases. Weight loss isn’t a treatment on its own - but combined with exercise and bracing, it makes all of them work better. Even small, consistent weight loss improves mobility and reduces inflammation.
When should I consider surgery?
Surgery (like total knee replacement) is usually considered only if you’ve tried at least 6 months of non-surgical options - bracing, exercise, injections, weight loss - and still have severe pain that limits daily life. If you can’t walk a block, sleep through the night, or stand up from a chair without help, it’s time to talk to an orthopedic surgeon. But remember: surgery has its own risks and recovery time. Most people who delay surgery and optimize non-surgical care end up needing it later - but with better outcomes.




11 Comments
Shirou Spade
November 24, 2025 AT 16:08 PMIt's funny how we treat pain like an enemy to be silenced, not a signal to be understood. Braces shift load, injections mute noise, but exercise? Exercise teaches your body it's still capable. The real cure isn't in a device or a needle-it's in showing up, day after day, even when it sucks. We want quick fixes because we've forgotten how to be patient with ourselves.
Lisa Odence
November 26, 2025 AT 12:31 PMAs a board-certified rheumatologist with over 27 years of clinical experience and a Ph.D. in Biomechanical Engineering from MIT, I must emphasize that the data presented here is statistically significant but lacks longitudinal follow-up beyond 12 months. Furthermore, the cited FDA approvals for hyaluronic acid formulations must be contextualized within the 2023 OARSI guidelines, which still classify intra-articular injections as conditionally recommended for patients with moderate-to-severe radiographic OA (Kellgren-Lawrence grade III/IV) who have failed conservative management. Additionally, the efficacy of PRP remains inconclusive due to heterogeneity in preparation protocols (e.g., leukocyte-rich vs. leukocyte-poor), and the cost-benefit ratio is not favorable in most U.S. healthcare systems without private insurance coverage. 🤔💉📊
Leisha Haynes
November 26, 2025 AT 17:57 PMExercise is the only thing that actually works but nobody wants to do it because it's hard and slow and you have to be accountable to yourself instead of blaming your doctor for not giving you a magic shot 🙄
Meanwhile I'm over here doing heel slides on my living room floor at 6am while my neighbor's dog barks at the mailman and wondering why I'm the only adult who didn't give up
Arup Kuri
November 27, 2025 AT 12:45 PMThey don't want you to know this but braces are just a distraction so you keep paying for pills and injections while Big Pharma owns the orthotists and the insurance companies and the FDA is just a puppet for the drug lords
Exercise? Nah they don't make money off that
They want you weak so you keep coming back
And don't get me started on those smart braces with sensors-totally tracking your movements for the government or the insurers
They're watching you move
They're watching you suffer
They're waiting for you to break
Andrew McAfee
November 29, 2025 AT 11:32 AMBack home in Kerala, we've been doing this for generations-warm oil massages before sunrise, slow walks along the riverbank, coconut oil on the knees, and never skipping the morning stretch. No braces. No shots. Just discipline and community. The West overcomplicates everything with gadgets and dollars. Sometimes the oldest solutions are the truest ones.
And yes, we still do it even when it rains.
Patricia McElhinney
November 30, 2025 AT 16:28 PMActually the entire premise of this article is dangerously misleading because it ignores the fact that 78% of knee OA patients in the US are obese and the real issue is systemic inflammation driven by processed carbs and sugar-not biomechanics. You can brace all you want but if you're still eating donuts and soda you're just delaying the inevitable. And don't even get me started on how lazy Americans are. You want relief? Stop being a couch potato and get your ass off the sofa. It's not rocket science. It's called basic human responsibility. #WakeUpAmerica
Agastya Shukla
December 1, 2025 AT 07:24 AMFrom a biomechanical standpoint, the SUCRA values referenced for bracing (92.1%) are derived from network meta-analyses with high heterogeneity in outcome measures. The 32.5% long-term improvement with exercise aligns with the 2022 Cochrane review, but the effect size is moderated by adherence rates, which are indeed suboptimal. Notably, the inclusion of neuromuscular training-particularly proprioceptive drills and eccentric loading-yields significantly higher functional gains than traditional strength protocols alone. I'd recommend integrating balance board work and single-leg stance drills post-PT. Also, the new FDA-approved hyaluronic acid formulation (Visco-3) demonstrates a 19% higher retention time in synovial fluid than prior iterations, though cost remains prohibitive for uninsured populations.
giselle kate
December 1, 2025 AT 23:50 PMWhy do we keep listening to these so-called experts? In my country, we don’t need fancy braces or $1,200 shots. We walk. We squat. We carry water. We lift our own groceries. We don’t sit on our butts waiting for someone to fix us. This whole medical-industrial complex is built on keeping us dependent. America’s weakness isn’t in its knees-it’s in its spirit. You think a sensor in your brace is going to save you? Wake up. Real strength doesn’t come from a device. It comes from refusing to quit.
Shivam Goel
December 2, 2025 AT 22:15 PMLet’s break this down statistically: The 30-45% pain reduction with bracing? That’s based on WOMAC scores, which have a known ceiling effect in high-functioning populations. The 82% 5-star Amazon review rate? That’s selection bias-only the satisfied buy and review. The 47% 1-star? That’s the real signal: 1 in 2 people hate the bulk, the heat, the chafing. And the exercise stats? 28.7% pain reduction? That’s a 2.1-point drop on a 10-point VAS. Clinically significant? Maybe. Meaningful? Only if you’re not in pain anymore. But let’s not pretend this isn’t a numbers game dressed up as hope. The real win? The placebo effect. And the real cost? Time. And dignity.
Amy Hutchinson
December 4, 2025 AT 21:17 PMokay but what if you're 70 and your knees hurt just to get out of bed and you have no money for a brace and your insurance denied the injection and your physical therapist quit because they got a better job and you live alone and your daughter works two shifts and you're too tired to do the exercises but you still want to hold your grandbaby without crying
what then
Jefriady Dahri
December 6, 2025 AT 03:11 AMHey, I’ve been there. Knee pain so bad I couldn’t play with my kids. Started with 10 minutes a day-just straight leg raises on the floor. No fancy gear. Just me, my mat, and my stubbornness. Took 3 months to feel real change. Now I hike. I dance. I lift my grandkids without wincing.
It’s not about perfection. It’s about showing up-even when you’re tired. Even when it hurts. Even when no one’s watching.
You got this. And if you need someone to cheer you on-I’m here. 💪❤️