Why Controller Medications Matter: The Real Deal for Asthma Control
Ever wondered why your doctor keeps reminding you about daily asthma meds, even when you feel fine most days? Here’s the kicker: long-term asthma controller medications do way more than stop a wheeze—they retrain your lungs to stay calm even when life throws triggers your way. Rescue inhalers (like albuterol or Ventolin) help in a crisis, but relying on them too often is usually a red flag. Your airways may be quietly inflamed, setting you up for surprise flares. That’s where controller therapies step in: they target airway inflammation at the source, so you aren’t reaching for your rescue inhaler every time you walk past a dog or the pollen count spikes.
It’s not a small issue. Data from the CDC shows that about 60% of people with asthma use rescue inhalers more than they realize, sometimes missing the creeping daily inflammation in their airways. Every puff of a controller inhaler is like sending in tiny firefighters to hose down inflammation before it smolders into an attack. If you need your rescue inhaler twice a week or more, most guidelines say that's a sign you need to revisit your daily controller plan.
So, let’s break down the players: inhaled corticosteroids (ICS), long-acting beta agonists (LABA), long-acting muscarinic antagonists (LAMA), and the new-generation biologic therapies. Each works with a specific target, and knowing how to use them right (plus a few dosing tricks) can mean breathing easy, even when life isn’t calm.
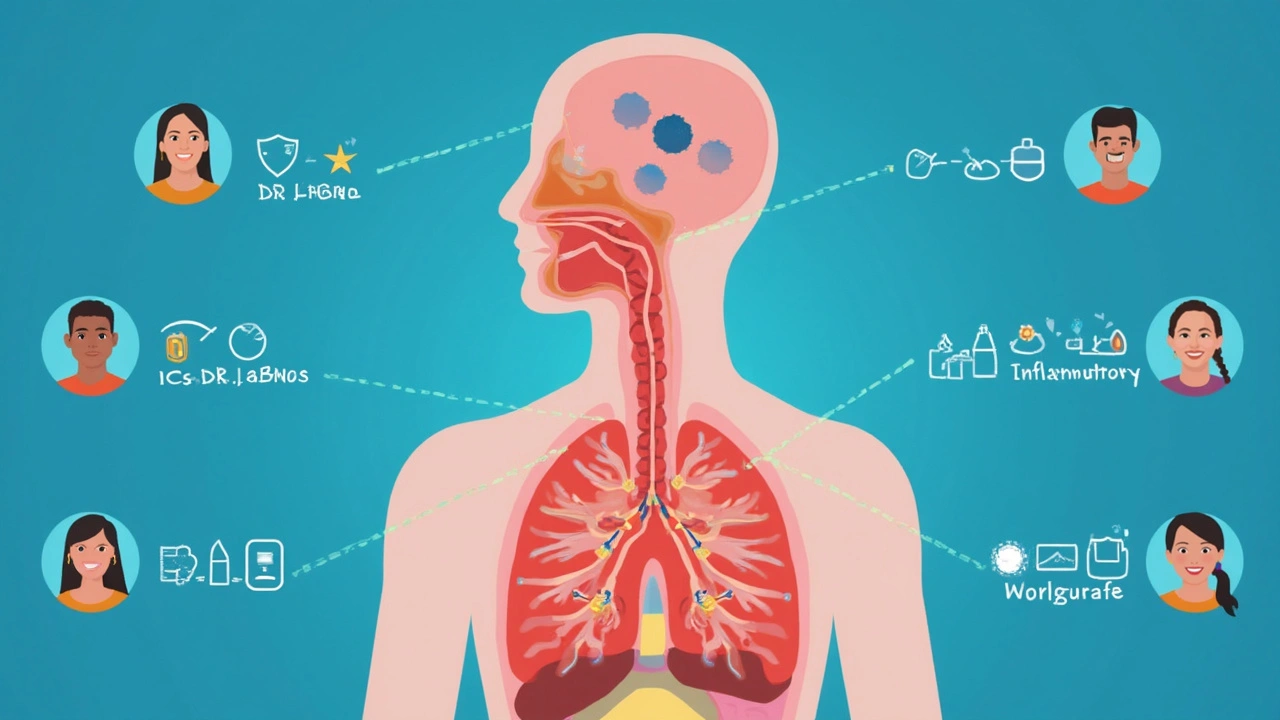
ICS, LABA, LAMA: How They Work & Smart Dosing Tips
Let’s start with inhaled corticosteroids (ICS). These are the backbone for most asthma plans. Fluticasone, budesonide, beclomethasone—different names, same principle. They tone down the chronic swelling in your lungs. Here’s a vital tip: ICS inhalers work best when you take them every day, even if you’re feeling fine. Miss doses, and inflammation slowly creeps back. Pairing with a spacer helps get more medicine deep into your lungs—less sticking to your mouth, less waste.
People sometimes think, “Won’t steroids thin my bones or affect my growth?” Good question. Inhaled steroids are way safer and lower-dose than oral ones. Decades of studies (like the CAMP trial) found that daily ICS use in kids only slightly slows growth in the first year, then kids catch up—much less concerning than repeated hospital visits for poorly controlled asthma. With adults, the risks are minor if you use the lowest dose that keeps you stable. Best tip? Rinse your mouth after using ICS to dodge thrush, a pesky mouth infection.
Next up: long-acting beta agonists (LABA). Think salmeterol or formoterol. LABAs relax the smooth muscle lining your airways and keep them open for up to 12 hours. They’re not quick fixes; they work slowly, so don’t use them for sudden symptoms. Combo inhalers (like Advair or Symbicort) often pair an ICS with a LABA, making it easier to stick to one inhaler. A fact you might not hear much: formoterol kicks in a bit faster than salmeterol, so some docs let you use Symbicort for both daily control and as needed, “mart” style—maintenance and rescue therapy.
What about LAMAs? Tiotropium is the big name here. This med blocks acetylcholine, a chemical that tightens airways. Adding a LAMA can benefit folks with severe or stubborn asthma who aren’t well-controlled on ICS/LABA alone. It usually comes in an inhaler you use once daily, but here’s a dosing trick: Always exhale fully before inhaling the medicine, and hold your breath after a slow, deep puff. That simple move can increase lung deposition by as much as 20% compared to a rushed inhale. Plus, LAMAs sometimes dry out your mouth, so keep water handy.
Ever wondered why some people take combo inhalers but still need their blue (rescue) inhaler often? Maybe their dose is too low, or they’re missing doses. Sometimes it’s technique: a review of asthmatic patients in primary care found over half did their inhaler steps out of order. Smart fix: have your doctor or pharmacist check your inhaler skills yearly.

Biologic Therapies and Personalized Asthma Control
Now, let’s talk about the big game-changer: biologic therapies. These are lab-designed antibodies that target specific parts of the immune response. For people with moderate-to-severe asthma—especially if you have lots of hospital visits, high eosinophil counts, or allergy-driven symptoms—biologics can mean fewer attacks and less need for oral steroids (which, honestly, nobody likes).
Omalizumab (Xolair), mepolizumab (Nucala), benralizumab (Fasenra), and dupilumab (Dupixent) are some top names. Each blocks a unique link in the allergic or eosinophilic inflammation chain. Dosing? Biologics are usually shots given every 2-8 weeks, depending on the drug and your body weight or specific blood work. Most are given at the doctor’s office, but some now allow self-injection at home—perfect for cutting down on clinic trips if you’re comfortable with a little needle action.
Worth noting: These meds aren’t for run-of-the-mill asthma. Doctors usually check for markers like IgE or eosinophil levels, and insurance wants you to have failed standard inhalers first. But the impact can be huge. In a 2023 real-world trial, patients on biologics saw ER visits drop by more than half in the first year. Some even stopped needing daily ICS altogether—though most keep a rescue inhaler around “just in case.” Side effects are low, but always look out for new rashes, headaches, or, rarely, allergic reactions.
If you’re seeking other options because you can’t tolerate inhalers, or want to see what else is out there, you might find some surprising ideas in this ventolin alternatives guide. It dives into different therapies, breathing exercises, and even over-the-counter choices with evidence behind them.
Here’s a quick run-down if you want to remember what matches your asthma:
- If you need a rescue inhaler several times a week, talk to your doctor about starting or stepping up an ICS (with or without a LABA/LAMA).
- If you’re on maximum inhaled meds and still struggling, ask if blood work could show you’re a candidate for biologics.
- Pay attention to inhaler skills. Even long-term asthmatics often miss little steps that limit medicine delivery.
- Try using a spacer with your ICS or ICS/LABA, especially if you notice powder on your tongue after inhaling. That’s medicine that didn't make it!
It can be easy to forget that asthma control is never one-size-fits-all. Weather, air quality, stress, and colds can all push your symptoms around—and sometimes just tweaking your daily meds keeps you two steps ahead. But the best tip? Check back in with your asthma action plan every few months. Bodies change, triggers shift, and your controller meds should keep up with you.




6 Comments
Scott Swanson
April 30, 2025 AT 00:50 AMOh sure, keep popping that blue puff like candy and pretend you don’t need a daily controller – what could possibly go wrong?
Every time you reach for rescue you’re basically shouting, “I don’t trust my own lungs!”
But guess what, the real heroes are the inhaled steroids that work quietly while you sleep, and they don’t need a shout.
Karen Gizelle
May 4, 2025 AT 02:53 AMIt is indefensible that anyone would ignore the strong evidence supporting daily inhaled corticosteroids. The only excuse I can imagine is a profound misapprehensionof the data.
Studies have repeatedly shown that consistent use reduces exacerbations and improves quality of life, yet some still cling to the myth that “I feel fine, so I don’t need it.”
Let us be clear: feeling fine today does not guarantee the same tomorrow.
Stephanie Watkins
May 8, 2025 AT 18:00 PMProper inhaler technique can make a huge difference in medication delivery.
Using a spacer, rinsing your mouth after an ICS dose, and timing your breath hold for at least ten seconds are simple steps that many overlook.
Even a modest improvement in deposition can translate to better control and fewer rescue puffs.
Zachary Endres
May 14, 2025 AT 07:20 AMImagine waking up every morning knowing that your lungs have already been armed with a silent squad of anti‑inflammatory warriors.
The beauty of a consistent ICS schedule is that it snuffs out the microscopic fires of inflammation that would otherwise erupt into full‑blown attacks.
When you pair that foundation with a LABA, you gain a reliable breeze that keeps your airways open for hours on end.
Adding a LAMA on top of the combo is like installing a reinforced dam, preventing the last stubborn contractions from spilling over.
For those whose asthma refuses to be tamed, biologics act as precision‑guided missiles, hunting down the exact immune pathways that fuel the chaos.
The data from recent real‑world studies show that patients on dupilumab or mepolizumab experience up to a 60 % reduction in emergency visits.
Because the reduction in exacerbations translates directly into fewer rescue inhaler puffs, your daily life becomes noticeably smoother.
But no therapy works miracles without proper technique; a missed step at the mouthpiece can waste up to half of the medication.
A quick spacer check, a thorough rinse, and a slow, deep inhalation can boost lung deposition by a full twenty percent.
Seasonal pollen, a cold, or even stress can still tip the balance, which is why a written asthma action plan is essential.
Review that plan with your clinician every three to six months, and adjust the dose before the symptoms become obvious.
Remember, the goal isn’t just to survive each flare, but to thrive with lungs that feel as free as a breezy day on the coast.
Your rescue inhaler should feel like a safety net, not a crutch you lean on multiple times a week.
Commit to the daily controller, practice your inhaler steps, and you’ll find that the blue can stay safely in the drawer.
In short, consistency, precision, and a dash of modern biology are the trio that can finally give you the breath of confidence you deserve.
Ashley Stauber
May 14, 2025 AT 08:43 AMWhile the hype around biologics is loud, many patients do just fine with optimized inhaler therapy and never need a pricey injection.
The American healthcare system already strains under the weight of unnecessary premiums, and adding another premium‑priced drug only deepens the divide.
Amy Elder
May 14, 2025 AT 10:06 AMGreat tips