Why switching to generic meds can backfire - even when they’re identical
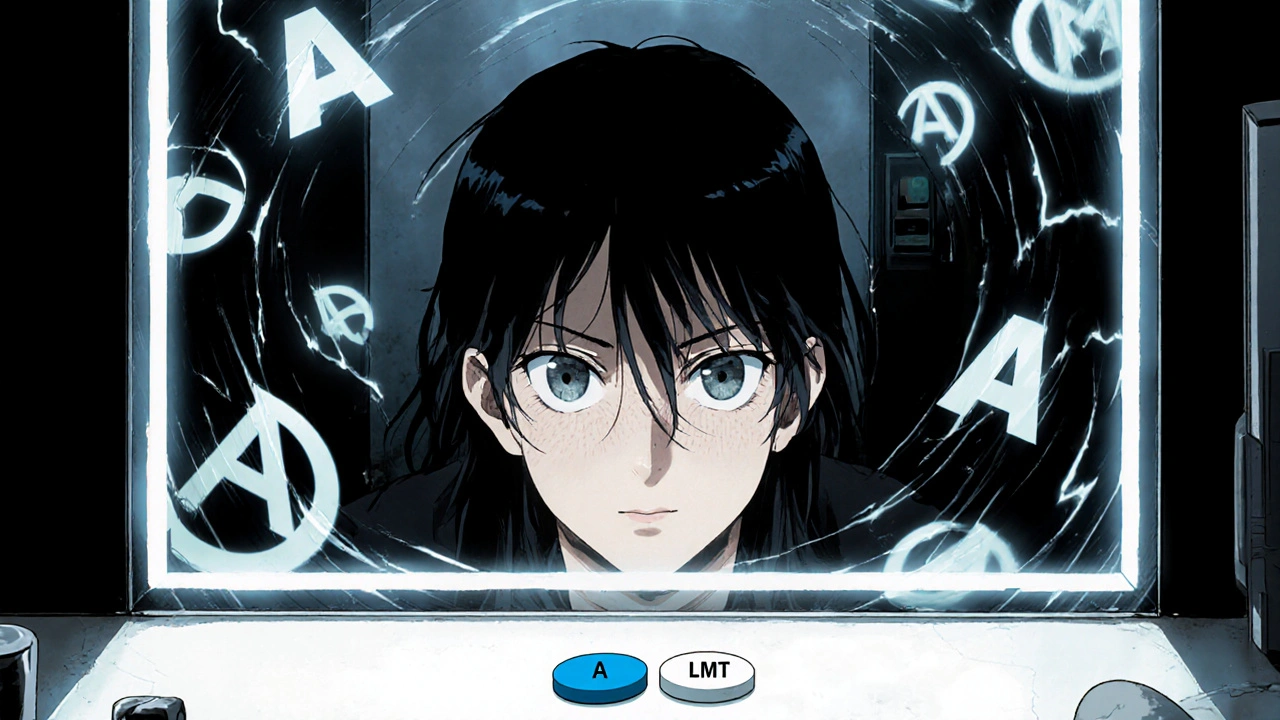
You’ve been taking your blood pressure pill for years. It’s the blue oval with the "A" stamped on it. Then one day, your pharmacy hands you a white round pill with "LMT" on it. Same dose. Same active ingredient. But suddenly, you feel different. Maybe you’re more tired. Maybe your headache’s back. You start skipping doses. You’re not alone.
Over 90% of prescriptions in the U.S. are filled with generic drugs. They save patients and insurers billions every year. But here’s the problem: medication adherence often drops after a brand-to-generic switch - not because the medicine doesn’t work, but because patients think it doesn’t.
Studies show that when people switch to generics, up to 19% more stop taking their meds altogether. For antidepressants, the drop is even worse. In one study, patients reported 18% more pain and 32% more side effects - even when the pill was just a placebo labeled as generic. This isn’t about chemistry. It’s about perception.
What’s really different between brand and generic drugs?
The FDA requires generics to match brand-name drugs in active ingredients, strength, dosage form, and how they’re absorbed. Bioequivalence is measured by two key numbers: Cmax (how fast the drug hits your bloodstream) and AUC (how much of it gets absorbed). The allowed range? 80% to 125% of the brand’s numbers. That’s the same variation you’d see between two batches of the same brand-name drug.
So why do people notice a difference? It’s not the active ingredient. It’s the rest.
- Inactive ingredients: Fillers, dyes, coatings. These don’t affect how the drug works, but they can trigger allergies in 3.7% of people - especially with skin reactions.
- Pill shape and color: A University of Michigan study found 28.4% of older adults get confused when their pill changes appearance. One man stopped taking his thyroid med because his new pill was "too small" - even though it was the same dose.
- Packaging: Different bottle labels, different blister packs, different instructions. All of it adds to the feeling that something’s wrong.
For most drugs, this doesn’t matter. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or seizure meds - even tiny shifts in absorption can matter. A 2017 study in the New England Journal of Medicine found a 0.8% higher hospitalization rate after switching these drugs to generics. Not because generics are unsafe. But because the margin for error is razor-thin.
Not all medications are the same when switching
Generic switches don’t affect everyone the same way. The impact depends on the drug class.
- Statins (cholesterol meds): Adherence goes up after switching. Why? Because the copay drops from $80 to $10. People take them more regularly when they’re affordable.
- Antihypertensives (blood pressure): Adherence drops by 12%. Patients report feeling "not the same," even though their blood pressure readings stay stable.
- Antidepressants: The worst case. Discontinuation rates jump 19.4%. People blame the generic for mood swings, fatigue, or anxiety - even when studies show no chemical difference.
- Diabetes and seizure meds: No major change in adherence. But that doesn’t mean there’s no risk. A class-action lawsuit against Teva in 2021 involved over 8,000 patients who reported seizures after switching from Lamictal to generic lamotrigine. The FDA found no bioequivalence issue - but the fear stuck.
The pattern? When cost is the main barrier, generics help. When trust is the barrier, generics hurt.
Why patients don’t trust generics - even when they should
Despite decades of FDA oversight, 62% of Americans still believe brand-name drugs are more effective. Why?
Marketing. Brand-name companies spend billions on ads that show happy, healthy people taking their pills. Generics? They show a pill in a bottle with a barcode. No emotion. No story.
Then there’s the "nocebo effect" - the opposite of placebo. If you expect a drug to cause side effects, your brain makes it happen. In a 2014 double-blind study, patients given identical placebo pills were 22% more likely to report side effects if they were told it was a generic.
And let’s not forget the pharmacy experience. In 2022, only 19% of patients were asked if they had concerns during a generic switch. Most just got a new pill and left.
What works: Best practices for keeping patients on track
Switching to generics doesn’t have to mean dropping adherence. Here’s what actually helps.
1. Talk to patients - really talk
Pharmacists have the most direct contact. But most transitions happen in under 90 seconds. That’s not enough.
Effective counseling takes 3.7 minutes - minimum. It needs to cover four things:
- Explain bioequivalence: "This generic has the same active ingredient and works the same way. The FDA requires it to be just as effective."
- Address appearance changes: "I know this pill looks different. That’s because the manufacturer changed the shape and color. But the medicine inside is the same."
- Highlight cost savings: "You’re saving $70 a month. That’s $840 a year."
- Invite questions: "What worries you about this change?"
When pharmacists do this, adherence jumps 31% - according to a 2022 meta-analysis.
2. Use technology to flag risky switches
E-prescribing systems can now automatically flag brand-to-generic switches for high-risk drugs like warfarin or levothyroxine. When this happens, the pharmacist gets a pop-up reminder to counsel the patient. In one study, this led to a 22.4% increase in adherence.
3. Synchronize refills
Patients on multiple meds often miss doses because refills are on different days. Medication synchronization - where all prescriptions are set to refill on the same date - improves adherence by 18.3% for generic users. It’s simple, cheap, and works.
4. Use pill organizers
When pills look different, confusion follows. A 2023 Kaiser Permanente study found that 63% of patients who used pill organizers reported better adherence after switching. Label the compartments with the drug name and condition - not just "morning" or "night."
5. Stick with the same manufacturer when possible
Generics from the same manufacturer are more likely to look and feel the same. If you’re on a critical drug like levothyroxine, ask your pharmacist: "Can I get the same generic brand as last time?" Many pharmacies can accommodate this.

What’s changing - and what’s coming
The FDA just announced a new rule: starting January 1, 2025, all generic manufacturers must include transition-specific patient education materials with their products. That’s a big step.
The Generic Pharmaceutical Association is also launching a "Seamless Switch" certification program. It will reward manufacturers who keep pill appearance consistent for high-risk drugs. That could cut confusion by half.
And AI is stepping in. Tools like AiCure use smartphone cameras to verify patients are taking their pills. In trials, they boosted adherence by 37% during generic switches.
But the biggest change? The Inflation Reduction Act caps out-of-pocket drug costs at $2,000 a year for Medicare patients. That means cost won’t be the main driver of non-adherence anymore. Now, the focus shifts to trust.
What patients should do
If you’ve been switched to a generic and feel off:
- Don’t stop taking it. That’s the worst thing you can do.
- Write down what you’re feeling: fatigue, headache, mood changes, nausea.
- Call your pharmacist. Ask: "Is this the same medicine I was on?"
- Ask your doctor: "Could this be a nocebo effect? Or should we switch back?"
Most of the time, your symptoms are psychological. But if they persist for more than two weeks, talk to your provider. There might be a reason - like an allergy to a filler - that needs attention.
What providers should do
Don’t assume patients understand generics. Don’t assume they’re fine just because they didn’t say anything.
- Use simple language: "This is the same medicine, just cheaper."
- Ask: "Have you taken this kind of pill before?"
- For high-risk drugs, document the switch in the chart and flag it for follow-up.
- Offer to check in two weeks after the switch.
Adherence isn’t about pills. It’s about trust. And trust is built one conversation at a time.





7 Comments
Josh Zubkoff
November 20, 2025 AT 20:12 PMOkay so let me get this straight - we’re telling people that a white pill with LMT on it is literally the same as the blue A-pill they’ve been taking for 12 years, but then we act shocked when they panic? This isn’t science, this is psychological warfare disguised as healthcare economics. I’ve seen patients cry because their antidepressant changed color. Not because it didn’t work - because it looked like a different drug. And don’t even get me started on the pharmacy tech who just slides the bottle across the counter like it’s a vending machine snack. No explanation. No empathy. Just ‘here’s your cheaper version, good luck.’ The FDA can say ‘bioequivalent’ all day, but when your brain is wired to associate pill shape with safety, you don’t care about statistical ranges. You care about the fact that your anxiety came back the moment you swallowed that tiny white thing. This isn’t about cost savings. It’s about control. And we’re taking it away from people without even asking.
fiona collins
November 21, 2025 AT 07:08 AMInteresting post. Thank you for the detailed breakdown.
Rachel Villegas
November 22, 2025 AT 19:40 PMThe part about pill organizers stood out to me. I’ve been using one since my switch to generic levothyroxine, and honestly? It’s been a game-changer. I label each compartment with the condition - ‘hypothyroid’ in the morning slot, ‘BP’ in the evening - and now I don’t second-guess whether I took it. No more staring at the bottle wondering if I’m holding the right one. Also, asking the pharmacist for the same manufacturer? Genius. I’ve stuck with the same generic brand for two years now. No issues. Just consistency.
giselle kate
November 24, 2025 AT 11:15 AMLet’s be real - this whole generic thing is a corporate scam disguised as progress. The FDA is a puppet of Big Pharma and Big Pharmacy. They approve generics that are barely bioequivalent, then lie to us saying it’s ‘the same.’ Meanwhile, Medicare patients are getting ripped off while CEOs get bonuses. And now they want to slap patient education on the bottle like that’s going to fix decades of trust erosion? Wake up. This isn’t about ‘perception’ - it’s about deliberate deception. We’re being treated like cattle to be herded into cheaper pills so insurance companies can pocket billions. The real problem isn’t the pill color - it’s a system that values profit over people. And until we stop letting them get away with this, people will keep dying because they stopped taking their meds out of fear. This isn’t healthcare. It’s exploitation.
Emily Craig
November 25, 2025 AT 08:52 AMOMG I CAN’T EVEN WITH THIS LOL
My grandma switched to generic warfarin and started having nightmares about turning into a blueberry. She swore the pill was ‘poisonous now.’ I had to sit her down with a flashlight and show her the FDA website. She cried. I cried. We ordered her the same generic brand from the same manufacturer - the one with the blue capsule. She’s been stable for 8 months. The science says it’s the same. But her brain? It knows better. And honestly? Who are we to tell her she’s wrong? If her brain needs the blue capsule to feel safe - then let her have the blue capsule. Cost is not worth a mental breakdown. Also - AI camera apps that check if you’re taking your meds? That’s wild. But also kinda creepy. Like… are we now being watched by robots to make sure we don’t skip our pills? I’m not sure I’m ready for that future.
Karen Willie
November 26, 2025 AT 22:24 PMI’ve been a pharmacist for 18 years. I’ve seen this play out over and over. The key isn’t just explaining bioequivalence - it’s listening. One woman came in crying because her generic antidepressant made her feel ‘empty.’ She didn’t want to stop taking it - she just wanted to know why she felt like a ghost. We talked for 12 minutes. I asked her about her routine, her sleep, her stress. Turns out her husband had just left. The pill hadn’t changed. Her life had. We kept the generic - but we added counseling. Sometimes the pill is just a mirror. The real work happens after the bottle is handed over.
Shivam Goel
November 27, 2025 AT 07:35 AMInteresting data - but where’s the real-world evidence from India? In Mumbai, 95% of prescriptions are generics - and adherence is higher than in the U.S. Why? Because patients don’t have a choice. They can’t afford brand names. So they take what they’re given - and they don’t overthink it. No ‘nocebo effect’ - because there’s no alternative. Also - in India, pill appearance is standardized across manufacturers for critical drugs. No color changes. No shape changes. Why? Because the government mandates it. In the U.S., we have the resources to care about pill aesthetics - but we waste them on marketing, not patient safety. Maybe the answer isn’t more education - it’s regulation. Stop letting manufacturers change pill shapes. Period. End of story.