When you hear the word biosimilar, you might think it’s just another generic drug. But that’s not true. Monoclonal antibody biosimilars aren’t copies in the way aspirin or metformin are. They’re complex biological medicines made from living cells-like tiny protein machines designed to target specific disease signals in your body. And because they’re made from living systems, no two batches are exactly alike. Even the original product has natural variations. That’s why regulators don’t require them to be identical-they just need to be highly similar with no meaningful difference in safety or effectiveness.
What Makes Monoclonal Antibody Biosimilars Different from Generics?
Generics are simple. They’re small molecules, chemically synthesized, and chemically identical to the brand-name version. A generic ibuprofen tablet has the same atoms in the same arrangement as Advil. Biosimilars? They’re proteins. Big ones. Around 150,000 daltons-about 25 times heavier than insulin and over six times heavier than growth hormone. These proteins are folded, modified, and tagged with sugar molecules (glycans) in living cell cultures. Tiny changes in the manufacturing process-temperature, pH, cell line-can alter those sugar patterns. And those changes? They can affect how the drug works in your body.
The FDA and EMA both require biosimilar manufacturers to prove similarity through over 100 analytical tests. These include mass spectrometry to check protein structure, cell-based assays to measure biological activity, and immunogenicity studies to see if your immune system reacts differently. The goal isn’t perfection-it’s confidence. If a biosimilar performs the same way in clinical trials as the original, and shows no unexpected side effects, it gets approved.
Approved Monoclonal Antibody Biosimilars and Their Uses
There are now dozens of approved monoclonal antibody biosimilars in the U.S. and Europe. Most target cancer or autoimmune diseases-conditions that used to cost tens of thousands of dollars per year. Here are the big ones:
- Bevacizumab biosimilars (Avastin): Used for colorectal, lung, ovarian, and brain cancers. Six biosimilars are approved in the U.S., including Mvasi, Zirabev, and Vegzelma. They block VEGF, a protein that feeds tumor blood vessels.
- Rituximab biosimilars (Rituxan): Treats non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and rheumatoid arthritis. Truxima, Ruxience, and Riabni are all approved. They target CD20 on B-cells, shutting down abnormal immune activity.
- Trastuzumab biosimilars (Herceptin): For HER2-positive breast and stomach cancers. Six options exist, like Ogivri, Herzuma, and Kanjinti. They lock onto the HER2 receptor and stop cancer cells from growing.
- Infliximab biosimilars (Remicade): Used for Crohn’s disease, ulcerative colitis, and rheumatoid arthritis. Remsima became the first monoclonal antibody biosimilar in the U.S. to get interchangeable status in July 2023-meaning pharmacists can substitute it without a doctor’s note.
- Adalimumab biosimilars (Humira): The most prescribed biologic in the world. Over 14 biosimilars are in development or approved, including Hyrimoz, approved in September 2023. They block TNF-alpha, a key inflammation driver.
These aren’t just theoretical. In real-world use, switching from the original to a biosimilar has shown no drop in effectiveness. A 2022 study in JAMA Oncology tracked 1,247 patients who switched from Rituxan to Truxima. The response rates, side effects, and survival outcomes were statistically identical. The only difference? Cost dropped by 28% per cycle.
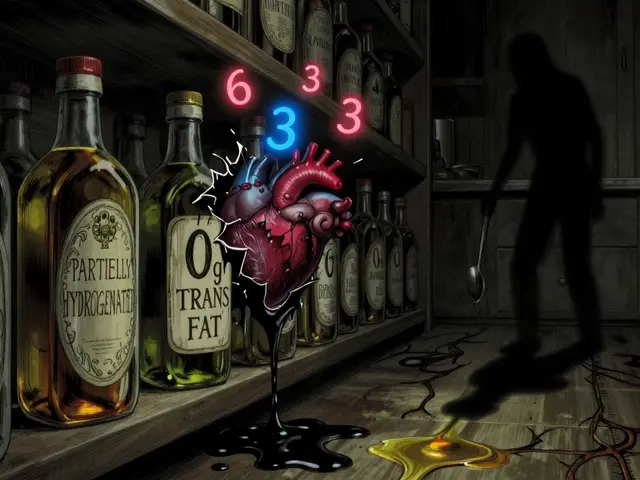
Why Cost Savings Matter
Biologics used to be among the most expensive drugs on the market. A year of Herceptin could cost over $70,000. Today, biosimilars sell for 15-35% less. In some cases, competition has driven prices down even further. The U.S. healthcare system could save $250 billion between 2023 and 2028 from monoclonal antibody biosimilars alone, according to Evaluate Pharma. That’s money that can be redirected to other patients, better infrastructure, or lower premiums.
But savings don’t happen automatically. Pharmacy benefit managers (PBMs) often control which drugs get covered. In 2023, 32% of biosimilar launches faced formulary restrictions-meaning insurers didn’t automatically include them. Providers need to actively choose them. And patients need to know they’re safe.

Safety and Immunogenicity: Real Concerns, Real Data
One big fear is immunogenicity-your body making antibodies against the drug. That can make it less effective or cause allergic reactions. The EMA’s 2021 safety report looked at 1.2 million patient-years of exposure to monoclonal antibody biosimilars. Only 12 cases of unexpected immune reactions were found. That’s 0.001%. The same rate was seen with the original products. So no, biosimilars aren’t riskier.
There was one famous case with cetuximab-an original antibody-where some patients had severe allergic reactions. It turned out they had pre-existing antibodies to a sugar molecule (alpha-1,3-galactose) found in the drug. That sugar came from the mouse cells used to make it. Biosimilar manufacturers now avoid those cell lines. They use human or engineered cells instead. The science has gotten smarter.
What’s Coming Next?
The pipeline is packed. As of September 2023, the FDA had 37 monoclonal antibody biosimilars in review. Six are targeting pembrolizumab (Keytruda), a leading immunotherapy for melanoma and lung cancer. If approved, these could bring down costs for checkpoint inhibitors-drugs that have revolutionized cancer care but remain out of reach for many.
Next up are even more complex molecules: bispecific antibodies (which target two proteins at once) and antibody-drug conjugates (antibodies carrying chemo directly to cancer cells). The EMA plans to release new guidelines for these in early 2024. The FDA is already updating its analytical standards, recommending 127 specific tests to map protein structure, charge variants, and glycosylation patterns. This isn’t guesswork anymore-it’s precision science.

Barriers to Widespread Use
Even with proven safety and cost savings, adoption is slow in some places. Why?
- Patent battles: Each biosimilar launch triggers an average of 14.7 patent challenges, according to UC Hastings. These lawsuits can delay market entry by years.
- Provider hesitation: A 2022 ASCO survey found only 58% of oncologists felt very confident prescribing biosimilars. Many still believe they’re "second-rate." But data doesn’t support that.
- Pharmacy confusion: Some pharmacists don’t know they can substitute interchangeable biosimilars without a new prescription. Education is lagging.
Change is happening, but it’s not automatic. Patients need to ask: "Is there a biosimilar for my drug?" Doctors need to feel supported in prescribing them. And insurers need to make them the default option.
Where This Is Headed
By 2027, monoclonal antibody biosimilars could make up 35% of all biologic prescriptions in the U.S., up from 18% in 2022. Cancer therapies will account for 62% of that volume. That means more people will get life-saving treatments-not just those who can afford $100,000-a-year drugs.
The future isn’t about replacing originals. It’s about expanding access. Biosimilars are the bridge between groundbreaking science and real-world affordability. They’re not perfect. But they’re close enough-and that’s enough to save lives.
Are monoclonal antibody biosimilars safe?
Yes. Regulatory agencies like the FDA and EMA require extensive testing to prove biosimilars have no clinically meaningful differences in safety, purity, or effectiveness compared to the original. Real-world data from over a million patient-years of use shows no increase in side effects or immune reactions. The safety profile is equivalent.
Can biosimilars be substituted for the original drug without a doctor’s approval?
Only if the biosimilar is designated as "interchangeable" by the FDA. As of 2023, Remsima (infliximab) is the first monoclonal antibody biosimilar with this status. Pharmacists can switch it for the original without notifying the prescriber. Most biosimilars are not yet interchangeable-so a new prescription is needed for each switch.
How much cheaper are biosimilars than the original biologics?
Biosimilars typically cost 15% to 35% less than the reference product. In some cases, competition has driven prices down further. For example, switching from Rituxan to Truxima cut costs by 28% per treatment cycle in a major U.S. cancer center study. Savings can reach hundreds of millions annually across health systems.
Do biosimilars work as well as the original drugs in cancer treatment?
Yes. Multiple clinical trials and real-world studies have confirmed that biosimilars for trastuzumab, rituximab, and bevacizumab perform just as well as the originals in treating breast cancer, lymphoma, and colorectal cancer. Response rates, progression-free survival, and overall survival are statistically identical.
Why aren’t more doctors prescribing biosimilars?
Some doctors lack confidence due to misinformation or limited training. A 2022 survey showed only 58% of oncologists felt "very confident" prescribing them. Others face pressure from pharmaceutical companies or are unsure about insurance coverage. Education and clear guidelines are improving this, but awareness still lags behind the evidence.
Are biosimilars available for all biologic drugs?
No. Biosimilars are only approved for biologics whose patents have expired or been legally challenged. Many newer drugs, like Keytruda and Humira, only recently became eligible. Over 37 monoclonal antibody biosimilars are in development, targeting newer agents. But for very recent biologics, biosimilars may still be years away.




10 Comments
Roshan Joy
January 10, 2026 AT 22:35 PMWhoa, this is actually one of the clearest explainers I’ve read on biosimilars. 🙌 I work in pharma logistics in India, and seeing these prices drop has been wild - my cousin just started on a trastuzumab biosimilar for breast cancer, and her out-of-pocket dropped from $800 to $550/month. Life-changing.
Michael Patterson
January 11, 2026 AT 17:33 PMOkay so let me get this straight - you’re telling me that a protein that’s 150,000 daltons can be "similar enough" but not identical and we’re just supposed to trust that? I mean come on, if I made a copy of my car engine and it had a 0.0003% variance in the piston coating, my mechanic would laugh me out of the shop. But somehow this is fine for drugs that go into people’s blood? 🤔 I’m not saying they’re bad, I’m just saying the science is so opaque it feels like a magic trick. Also, typo: "glycans" not "glycans" - wait no, that’s right. I’m confused now.
Matthew Miller
January 12, 2026 AT 12:42 PMLet’s be real - this whole biosimilar thing is just Big Pharma’s way of extending their monopoly by another 5 years while pretending to be altruistic. The "100+ analytical tests"? That’s just a checklist they wrote themselves. And don’t get me started on the "interchangeable" label - that’s a legal loophole dressed up as science. If you think these things are safe, you haven’t read the FDA’s own whistleblower reports from 2021. They’re playing you.
Madhav Malhotra
January 13, 2026 AT 03:24 AMAs someone from India, I’m so proud to see how biosimilars are making cancer care accessible here. My uncle got Rituximab biosimilar for lymphoma - cost was 1/5th of the original. The docs were nervous at first, but he’s been in remission for 2 years now. We don’t have the luxury of waiting for expensive drugs. Biosimilars aren’t just cheaper - they’re justice.
Priya Patel
January 14, 2026 AT 08:53 AMOMG I just read this whole thing and I’m crying?? Like, seriously - I have RA and was on Humira for 4 years. My insurance finally switched me to Hyrimoz last year and I was terrified. But guess what? I feel the SAME. No new rashes, no flares, and my co-pay went from $400 to $90. I’m telling all my support group members. This is the quiet revolution we didn’t know we needed 💕
Jason Shriner
January 14, 2026 AT 20:09 PMSo... we're now trusting protein molecules that are "close enough" because capitalism says so? Fascinating. I mean, if your therapist says you're "emotionally similar" to your ex, does that mean you can just swap them? 😏 The real biosimilar here is our collective willingness to trade certainty for convenience. Also, who approved this as a "medical breakthrough"? A VC?
Alfred Schmidt
January 16, 2026 AT 13:35 PMTHIS IS A SCAM. I’ve been on infliximab for Crohn’s for 11 years. I switched to Remsima last year because my insurer forced me. I had a flare-up within 6 weeks. They said "it’s placebo." But I know my body. And I’m not a lab rat. The FDA doesn’t test for long-term immune memory - they test for 12 weeks and call it a day. And now they’re calling it "interchangeable"?! I’m not interchangeable. My immune system isn’t a vending machine. I’m done with this.
Vincent Clarizio
January 17, 2026 AT 02:35 AMLook - I get the fear. I really do. But let’s not confuse the complexity of biology with the simplicity of our expectations. You can’t make a perfect copy of a snowflake - and you can’t make a perfect copy of a protein folded in a living cell. That’s not a flaw - that’s the nature of life. The fact that we can get within 99.9% similarity, validate it with mass spec, cell assays, and clinical outcomes, and still save billions? That’s not just science - it’s a moral triumph. And if you’re still skeptical, go read the JAMA Oncology study again. The data doesn’t lie. It’s just inconvenient for the fear-mongers.
Sam Davies
January 17, 2026 AT 23:46 PMHow quaint. The American healthcare system, ever the innovator, has found a way to make life-saving drugs cheaper by pretending they’re not actually different. How very… utilitarian. One wonders whether the EMA’s 1.2 million patient-years of data was peer-reviewed by a hedge fund or just a regulatory bureaucrat with a PowerPoint. Still, I suppose if you’re going to commodify biology, you might as well do it with a straight face.
Christian Basel
January 18, 2026 AT 01:36 AMTL;DR: Biosimilars = glycosylation variance + regulatory arbitrage + formulary leverage. The real bottleneck isn’t science - it’s PBM inertia and provider cognitive dissonance. The 28% cost reduction is real, but adoption curves are flat because of entrenched IP ecosystems and lack of clinical decision support integration. We need value-based contracting, not just price cuts. Also, the term "interchangeable" is misleading - it’s a regulatory category, not a clinical one. Fix the system, not the label.