Cost-Benefit Analysis in Medications: Weighing Risks, Costs, and Real-World Outcomes
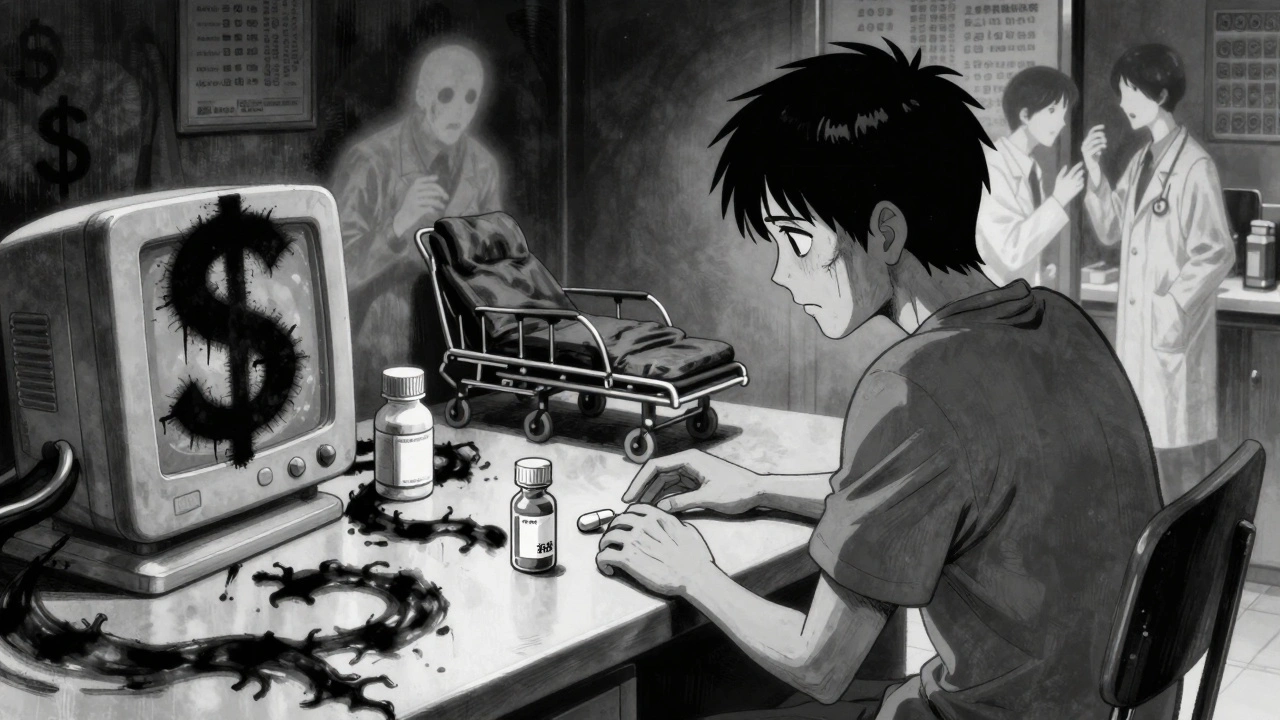
When you hear cost-benefit analysis, a practical method for comparing the financial and health outcomes of a medical decision, it’s not just for hospital administrators. It’s something you live every time you choose between a brand-name pill and a generic, decide whether to keep taking a drug that makes you drowsy, or wonder if that expensive injection is really worth it. This isn’t theory—it’s daily life for anyone managing chronic conditions, dealing with side effects, or trying to stretch a prescription budget.
It shows up in generic drugs, medications approved as equivalent to brand-name versions but sold at lower prices when a patient stops taking them because the pill looks different—even though science says it works the same. That drop in adherence? That’s a hidden cost. It’s also why drug interactions, when one medication changes how another works in the body matter. A proton pump inhibitor might cut your stomach acid, but if it makes your HIV meds useless, the savings vanish. And then there’s pharmacokinetics, how your body absorbs, moves, and breaks down a drug. Two drugs might have the same active ingredient, but if one hits peak concentration too fast or too slow, it could mean more side effects or less control. These aren’t just lab terms—they’re the invisible math behind every pill you swallow.
Cost-benefit analysis doesn’t just look at price tags. It weighs how often you forget to take your meds, whether a side effect ruins your sleep, if a cheaper option forces you to visit the ER more, or if a generic switch leads to confusion and missed doses. It’s why automated refills for generics help—because forgetting a refill isn’t just inconvenient, it’s a financial and health risk. It’s why skin testing for penicillin allergies matters: if you’re wrongly labeled allergic, you get pricier, less effective antibiotics. And it’s why switching from brand to generic isn’t just about saving money—it’s about keeping you on treatment long enough to actually get better.
What you’ll find below isn’t a list of abstract studies. It’s real stories from people who’ve faced these trade-offs: the diabetic who nearly lost control after drinking alcohol with their meds, the asthma patient who learned to cut pollution exposure with a $40 filter, the person who stopped statins out of fear—only to learn they might have lowered their ALS risk. These are decisions made under pressure, with incomplete info, and with real consequences. This collection gives you the facts to make smarter calls—not just cheaper ones.
Outcomes Economics: The Real Cost-Benefit of Using Generic Medications
Generic medications save billions in healthcare costs, but true value comes from improved adherence, fewer hospitalizations, and better long-term outcomes. HEOR reveals the real cost-benefit of generics beyond just price.




