Dental Anesthesia Risks – Essential Facts and Safety Tips
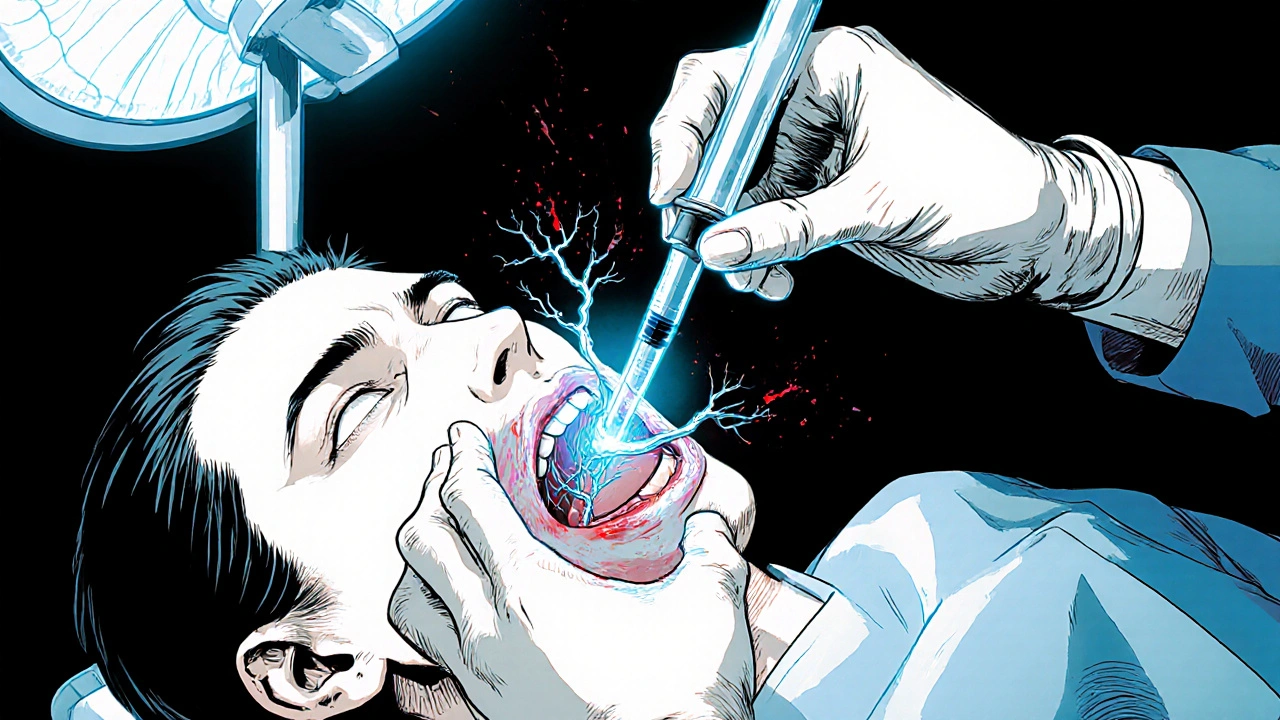
When dealing with dental anesthesia risks, the potential complications that can arise during or after the use of anesthetic agents in dental procedures. Also known as oral sedation complications, it is a concern for patients and clinicians alike. Key issues include local anesthetic toxicity, overdose or accidental intravascular injection causing systemic effects such as dizziness, seizures, or cardiac arrest, nerve injury, temporary or permanent loss of sensation after blocks like the inferior alveolar nerve injection, allergic reaction, immune responses ranging from mild rash to life‑threatening anaphylaxis, and cardiovascular complications, abnormal heart rate or blood pressure shifts triggered by certain anesthetic drugs. Understanding these entities helps you anticipate and prevent problems.
Dental anesthesia risks encompass a blend of drug‑related and technique‑related factors. For example, local anesthetic toxicity often stems from using high‑dose lidocaine without considering a patient’s weight or liver function, which is why a thorough medical history is mandatory. Nerve injury, on the other hand, is linked to needle placement; improper angle or depth can compress or stretch the nerve, leading to paresthesia. Allergic reactions influence the safety of dental anesthesia by dictating which agents are suitable—if a patient is known to be hypersensitive to vasoconstrictors, alternative formulations must be selected. Cardiovascular complications require real‑time monitoring because some agents, like epinephrine, can raise blood pressure, especially in patients with hypertension.
Common Types of Risks and How to Manage Them
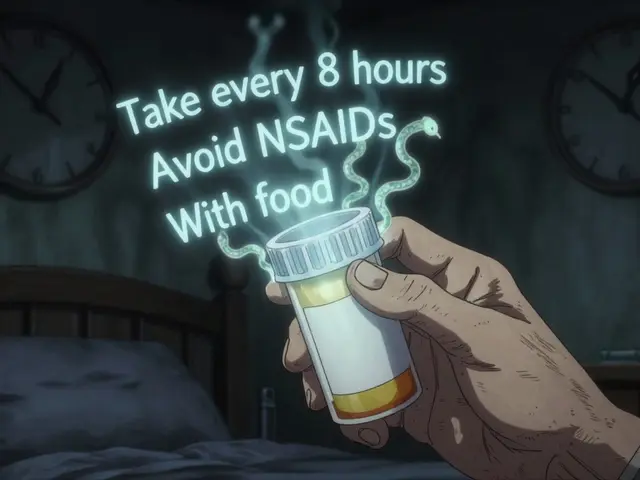
First, local anesthetic toxicity is prevented by calculating the maximum safe dosage based on body weight and adjusting for additives like epinephrine. Second, nerve injury is reduced by using proper injection techniques, employing short‑bevel needles, and avoiding excessive force. Third, allergic reaction risk drops when clinicians perform allergy screening and keep emergency medication (epinephrine auto‑injectors, antihistamines) on hand. Fourth, cardiovascular complications are managed by monitoring vital signs, selecting low‑dose vasoconstrictors, and consulting the patient’s physician if they have heart disease.
The articles below dive deeper into specific drugs and scenarios that intersect with dental anesthesia. You'll find comparisons of analgesics, antibiotics, and sedatives—information that helps you decide which medication fits a given dental case while keeping risks low. Whether you’re a patient curious about safety or a dental professional looking for quick reference, the collection offers practical insights you can apply right away. Below, explore each detailed guide to see how the concepts of toxicity, nerve injury, allergy, and cardiovascular effects play out in real‑world dental care.
Pros and Cons of Using Local Anesthesia in Cosmetic Dentistry
Explore the real advantages and drawbacks of using local anesthesia for cosmetic dental procedures, learn about common drugs, risks, and how to choose the best pain‑control plan for your smile.