Health Economics: How Drug Costs, Access, and Policy Shape Your Care
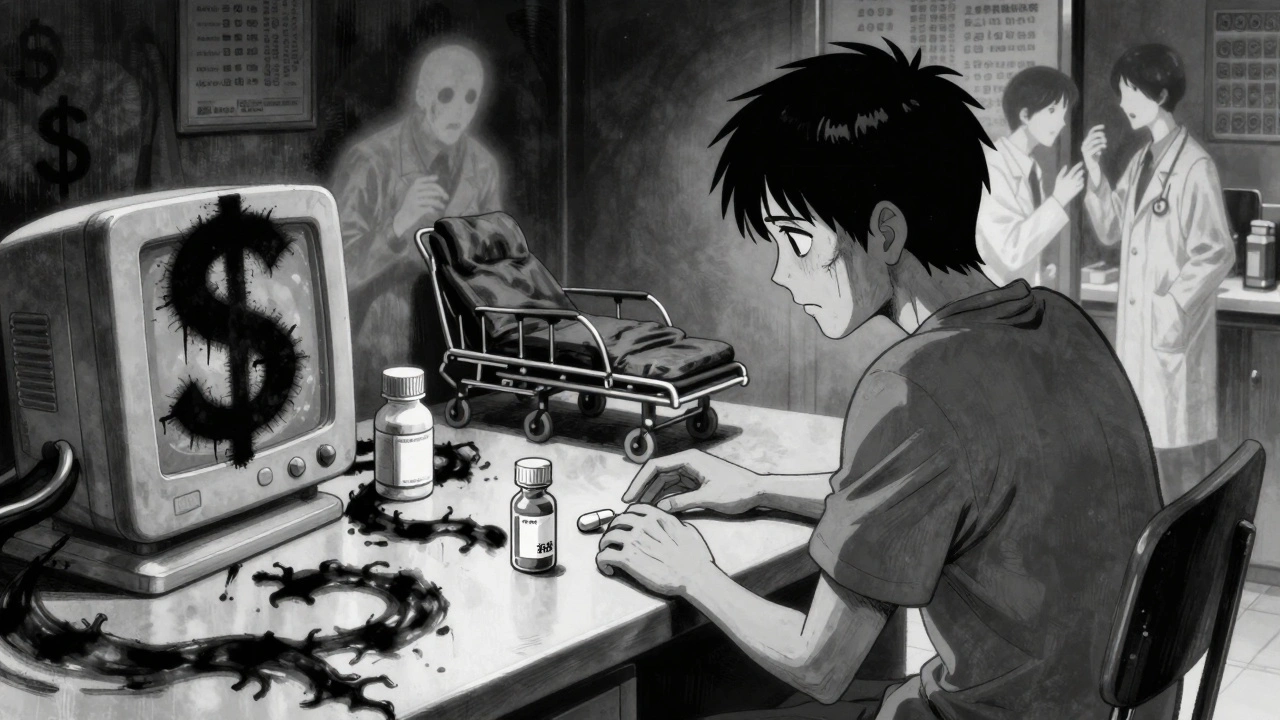
When you hear health economics, the study of how resources are allocated in healthcare, including drug pricing, insurance coverage, and patient access. Also known as medical economics, it’s not just about big pharma profits—it’s about why your prescription costs $500 one month and $15 the next, or why your doctor can’t prescribe the drug that works best for you. This isn’t theoretical. It’s why a generic version of your medicine sits on the shelf for years after the FDA says it’s safe—because of patent fights, manufacturing delays, or insurance gatekeeping.
generic medications, lower-cost versions of brand-name drugs that must meet the same safety and effectiveness standards. Also known as generic drugs, they’re the backbone of affordable care—but their rollout isn’t automatic. Look at the posts here: tentative approvals sit for years due to legal battles, pill appearance changes confuse patients, and automated refills help or hurt adherence depending on how they’re set up. These aren’t glitches—they’re outcomes of economic decisions. Meanwhile, drug pricing, how pharmaceutical companies set costs for medications, often based on market control rather than production expense. Also known as pharmaceutical pricing, it explains why a 30-day supply of a life-saving drug can cost more than a used car, while the same pill in another country costs a fraction. And it’s not just about the sticker price. It’s about what your insurance covers, whether you need prior authorization, and if your pharmacy even stocks the cheaper version.
Health economics doesn’t just affect your wallet—it affects your health. If you skip a dose because the co-pay is too high, that’s health economics in action. If your doctor switches you to a generic because your insurer won’t cover the brand, that’s health economics. If a new drug gets approved but takes two years to reach your local pharmacy, that’s health economics too. The posts below show you how these systems play out in real life: from statins and diabetes meds to skin creams and heart drugs. You’ll see how patent litigation delays generics, how switching brands messes with adherence, and how online pharmacies try to fix the system. This isn’t about politics—it’s about what you’re actually getting when you walk out of the pharmacy.
What you’ll find here isn’t a lecture on budgets or policy papers. It’s real stories from people who’ve been stuck between a high price and a failing treatment. It’s the why behind the pill you take—or don’t take. And it’s the hidden rules that decide whether your care works, or just costs too much to keep up with.
Outcomes Economics: The Real Cost-Benefit of Using Generic Medications
Generic medications save billions in healthcare costs, but true value comes from improved adherence, fewer hospitalizations, and better long-term outcomes. HEOR reveals the real cost-benefit of generics beyond just price.