Psychotropic Medication Weight Gain Calculator
How Your Medication May Affect Your Weight
This calculator estimates expected weight gain based on your current medication and weight. Remember: Weight gain from psychotropic medications is biological, not a lack of willpower.
The medical community defines medication-related weight gain as a 7% increase from your starting weight. For example, a 160 lb person would be considered at risk at 11 lbs gained.
Your Results
Enter your information to see your estimated weight gain.
When you start taking a psychotropic medication - whether it’s for depression, bipolar disorder, or schizophrenia - your doctor’s main goal is to help you feel better. But for many people, that improvement comes with an unexpected side effect: weight gain. It’s not just about clothes feeling tighter. This weight gain can raise your risk for diabetes, heart disease, and even shorten your life. The truth is, if you’re on medications like olanzapine, clozapine, or mirtazapine, gaining 5 to 10 pounds in the first few months is common. And if you’ve tried dieting before and failed, you’re not alone. Psychotropic drugs make losing weight harder than you’d expect.
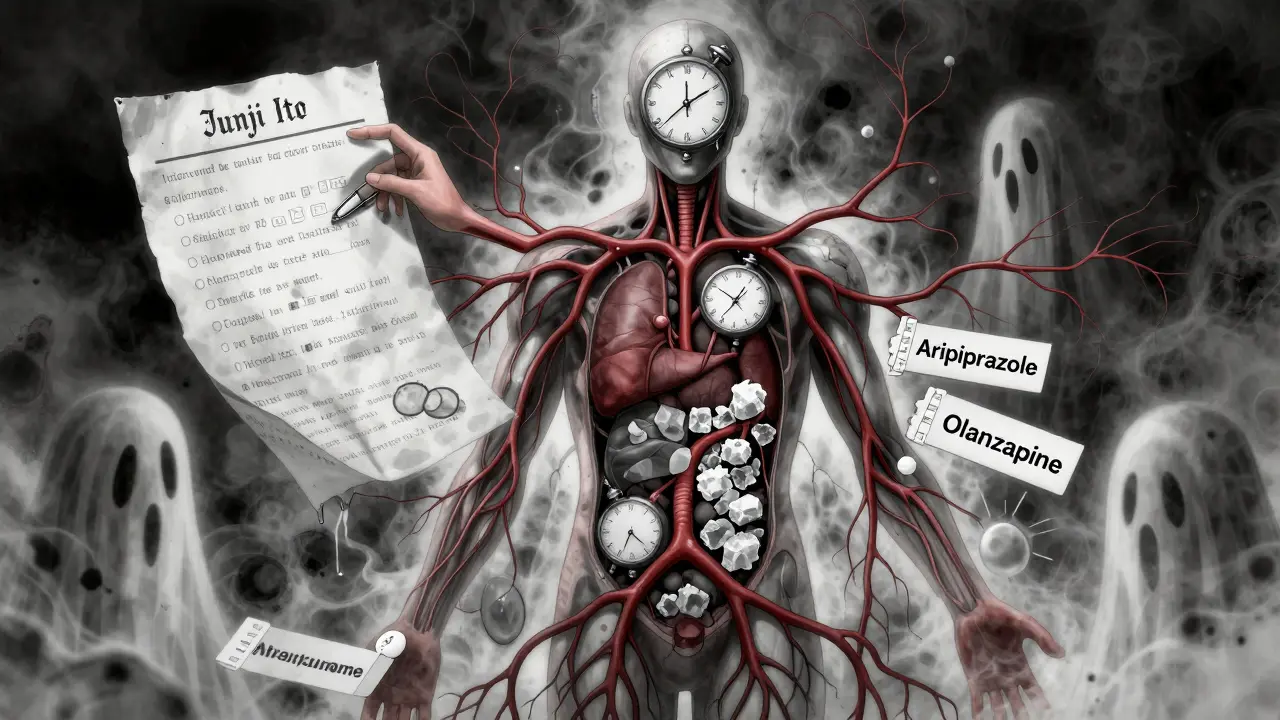
Why Do These Medications Cause Weight Gain?
It’s not because you’re eating too much or lazy. The weight gain is built into how these drugs work. Most psychotropics block certain receptors in your brain - especially histamine-1, serotonin-2C, and dopamine-2. These same receptors help control hunger, metabolism, and how your body stores fat. When they’re blocked, your appetite increases, your body burns fewer calories, and fat storage goes up. Some people feel constant hunger, even after eating. Others notice their body slows down its natural calorie-burning process.Not all drugs are the same. Clozapine and olanzapine are the biggest offenders. Studies show people on these medications gain an average of 4 kilograms (almost 9 pounds) in just 10 weeks. By the end of the first year, many gain over 10 kilograms. On the other end of the spectrum, lurasidone and aripiprazole cause almost no weight gain - sometimes less than placebo. Paliperidone is also relatively neutral over a full year. This difference isn’t small. It’s the difference between staying healthy and developing metabolic syndrome.
How Much Weight Gain Is Too Much?
The medical community defines medication-related weight gain as a 7% increase in body weight from your starting point. For someone who weighs 160 pounds, that’s 11 pounds. But even smaller gains matter. A 5% weight increase can already raise your blood sugar and cholesterol. The problem is, many people don’t notice the change until it’s too late. By then, insulin resistance is setting in, and your waistline is expanding.And it’s not just about weight. These drugs also affect your blood sugar, triglycerides, and blood pressure. Together, they create metabolic syndrome - a cluster of conditions that doubles your risk for heart disease and stroke. People with serious mental illness already live 10 to 20 years less than the general population. Weight gain from medications is one of the biggest reasons why.
Which Medications Carry the Highest Risk?
Here’s a quick breakdown based on real-world data:| Medication Class | Medication | Average Weight Gain (First Year) | Risk Level |
|---|---|---|---|
| Second-Generation Antipsychotics | Clozapine | 7-10 kg (15-22 lbs) | Very High |
| Second-Generation Antipsychotics | Olanzapine | 6-9 kg (13-20 lbs) | Very High |
| Second-Generation Antipsychotics | Quetiapine | 3-5 kg (7-11 lbs) | Moderate |
| Second-Generation Antipsychotics | Risperidone | 2-4 kg (4-9 lbs) | Moderate |
| Second-Generation Antipsychotics | Aripiprazole | 0-2 kg (0-4 lbs) | Low |
| Second-Generation Antipsychotics | Lurasidone | 0.5-1 kg (1-2 lbs) | Very Low |
| Antidepressants | Mirtazapine | 4-7 kg (9-15 lbs) | High |
| Antidepressants | Amitriptyline | 3-6 kg (7-13 lbs) | High |
| Antidepressants | Paroxetine | 2-4 kg (4-9 lbs) | Moderate |
| Mood Stabilizers | Lithium | 2-5 kg (4-11 lbs) | Moderate |
| Mood Stabilizers | Valproate | 3-6 kg (7-13 lbs) | Moderate to High |
First-generation antipsychotics like chlorpromazine and thioridazine can also cause weight gain, but they’re used less often now. Haloperidol, however, tends to be more neutral. Among antidepressants, mirtazapine and amitriptyline are the worst, while bupropion and sertraline are much safer choices. If you’re switching meds, this data matters.
Why Losing Weight Is So Hard on These Medications
You might think, “If I eat less and exercise more, I’ll lose the weight.” But research shows it’s not that simple. A 2016 study of over 800 people in a weight-loss program found that those taking psychotropics lost 1.6% less weight than those who weren’t. Only 31.8% of them hit the 10% weight loss goal - compared to 41.2% of people not on these drugs. Why? The medications alter your metabolism at a cellular level. They make your body hold onto fat, even when you’re in a calorie deficit. They also increase cravings for carbs and sugars. And if you’re dealing with fatigue, low energy, or depression, sticking to a workout routine becomes even harder.This isn’t about willpower. It’s biology.
What Can You Do About It?
There are three proven strategies - and the best approach often combines them.- Switch to a lower-risk medication - If your symptoms are stable, switching from olanzapine to aripiprazole or lurasidone can prevent further gain - or even reverse some of it. But this isn’t always safe. If you’ve been on a high-risk drug for years, changing it could trigger a relapse. Talk to your psychiatrist before making any moves.
- Add metformin - This diabetes drug has been studied in over 1,000 people on antipsychotics. It reduces weight gain by 2-4 kg compared to placebo. It also improves insulin sensitivity. It’s safe, cheap, and often covered by insurance. Many psychiatrists now prescribe it proactively.
- Use structured lifestyle support - Random advice like “eat less” doesn’t work. You need a plan. Weekly sessions with a dietitian who understands psychiatric meds, a tailored exercise routine that matches your energy levels, and meal planning that accounts for increased appetite can make a real difference. Programs that include a psychiatrist, dietitian, and fitness coach together see the best results.
Topiramate is another option - it can help you lose 3-5 kg - but it has side effects like brain fog and tingling. It’s not for everyone. And while newer drugs like GLP-1 agonists (think semaglutide) show promise in early trials, they’re not yet standard for psychiatric patients.
What the Experts Say
The American Psychiatric Association recommends checking your weight, waist size, and blood sugar every three months after starting a psychotropic. Many clinics don’t do this - but you should ask. If your weight goes up more than 5% in three months, don’t wait. Talk to your doctor. Don’t assume it’s normal.Dr. John Newcomer, a leading researcher, says: “Never trade one problem for another. You can’t control psychosis if you’re dead from a heart attack.” That’s why prevention matters more than reversal. The best time to act is before you gain the weight.
What’s New in 2026?
The field is moving fast. In 2021, the FDA cleared a digital tool called Moodivator - an app that tracks food, mood, and activity specifically for people on psychiatric meds. A 2022 trial showed users lost 3.2% more weight than those using standard methods. That’s not huge, but it’s meaningful.Genetic testing is also on the horizon. Researchers have found that people with certain variations in the MC4R gene are much more likely to gain weight on antipsychotics. Within the next few years, doctors may test for this before prescribing - so you won’t be put on a drug that’s likely to cause major weight gain.
And the VA, which treats over 9 million veterans, now requires quarterly metabolic screenings for everyone on antipsychotics. Since 2010, they’ve seen a 15% improvement in catching early signs of diabetes and fatty liver. That’s proof that structured monitoring works.
What You Should Do Right Now
If you’re on a psychotropic and worried about weight:- Ask your doctor: “What’s the weight gain risk of this drug?”
- Get your weight, waist size, and fasting glucose checked - baseline and every 3 months.
- If you’ve gained 5% or more, don’t wait. Ask about metformin.
- Find a dietitian who’s worked with psychiatric patients - they know how to handle increased appetite and low energy.
- Don’t stop your medication because of weight gain. Talk to your provider. There are safer options.
Weight gain isn’t your fault. But managing it is possible - if you act early, use the right tools, and work with a team that understands both your mind and your metabolism.
Can you lose weight while on antipsychotics?
Yes, but it’s harder. Weight loss requires more structure than usual. Studies show people on antipsychotics lose less weight in standard programs. Combining metformin, behavioral counseling, and tailored exercise can lead to meaningful loss - often 5% or more over 6-12 months. It takes time and support, but it’s achievable.
Which antipsychotic causes the least weight gain?
Lurasidone and aripiprazole cause the least weight gain - often less than 1 kg (2 lbs) over a year. Ziprasidone and asenapine are also low-risk. Paliperidone is close to neutral. These are good options if you’re starting treatment or considering a switch.
Does metformin help with weight gain from psychiatric drugs?
Yes. Multiple clinical trials show metformin prevents 2-4 kg of weight gain and can even reverse some of it. It improves insulin sensitivity, reduces cravings, and is generally well-tolerated. Many psychiatrists now prescribe it alongside antipsychotics, especially for high-risk drugs like olanzapine or clozapine.
Why do some people gain weight and others don’t on the same drug?
Genetics, metabolism, and lifestyle all play a role. Some people have gene variants (like MC4R) that make them more sensitive to the appetite-stimulating effects of these drugs. Others have higher baseline activity levels or better insulin sensitivity. It’s not about willpower - it’s biology. That’s why personalized approaches are becoming more important.
Should I stop my medication if I’m gaining weight?
No. Stopping psychiatric medication without medical supervision can lead to relapse, hospitalization, or worse. Instead, talk to your psychiatrist. There are safer alternatives, and strategies like metformin or lifestyle changes can help. Never make changes on your own.
Are there any new treatments on the horizon?
Yes. GLP-1 receptor agonists (like semaglutide) are being tested in psychiatric populations and have shown 5-8% weight loss in early trials. Digital tools like the FDA-cleared Moodivator app are already helping people track progress and stay on track. Genetic testing to predict weight gain risk is also in development - and could soon guide medication choices before they start.