Glaucoma is a silent thief of sight. Often going unnoticed until significant vision loss occurs, it remains a leading cause of irreversible blindness worldwide. The condition damages the optic nerve, which is crucial for vision. Early detection and continuous monitoring are key to managing its progression.
This is where optic nerve imaging steps in. By using advanced technologies, doctors can get detailed visuals of the optic nerve, allowing for accurate diagnosis and effective monitoring. These images help healthcare professionals determine the severity of the condition and monitor how it changes over time.
From Optical Coherence Tomography (OCT) to Scanning Laser Polarimetry (SLP) and beyond, several techniques are available. Each has its strengths, and often, they are used in combination to provide a comprehensive view of the nerve's health.
Understanding the results from these images can be complex, but it’s essential. Knowing what to look for and how to interpret these results can make a significant difference in managing glaucoma.
For patients, staying informed and following your eye care routine can make a world of difference. Maintaining regular check-ups, understanding the importance of each test, and adhering to treatment plans are vital steps in preserving vision.
- Understanding Glaucoma
- Importance of Early Diagnosis
- Technologies Used in Optic Nerve Imaging
- Interpreting the Results
- Patient Tips and Recommendations
Understanding Glaucoma
Glaucoma is not just one condition; it’s a group of eye disorders that damage the optic nerve and can lead to vision loss and blindness. One of the main causes of this damage is high intraocular pressure (IOP). However, even people with normal IOP can develop glaucoma. This makes it crucial to have regular eye check-ups to catch the disease early. Genes play a role too, with family history increasing the risk.
In its early stages, glaucoma often doesn’t show any symptoms. It's nicknamed the ‘silent thief of sight’ because damage occurs gradually, and you might not notice any changes until the condition is advanced. This is why understanding and recognizing the early signs is important. Some types of glaucoma, like acute angle-closure glaucoma, can appear suddenly and are considered medical emergencies. They might include severe eye pain, headache, nausea, and sudden vision loss.
The condition primarily affects the peripheral vision first, working its way to central vision if left untreated. This means that someone could lose a significant portion of their vision before realizing there’s a problem. Treatments can't restore vision lost, but they can help stop further damage. So, timely diagnosis and treatment are crucial. According to the World Health Organization, glaucoma is responsible for 12.3% of global blindness, which highlights its massive impact.
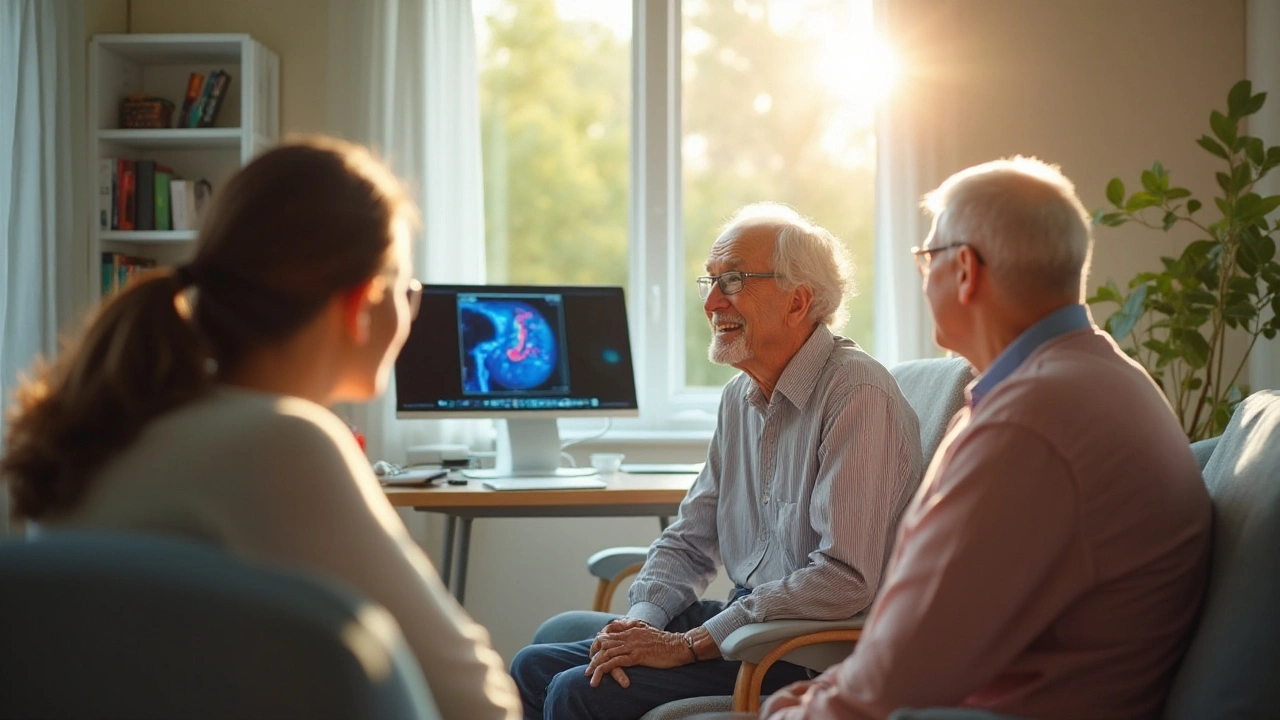
“It is essential to spread awareness and ensure that people go for regular eye exams,” says Dr. Jane Smith, an ophthalmologist. “Early diagnosis through tools like optic nerve imaging can save millions from losing their vision.”
There are different types of glaucoma. The two most common types are open-angle and angle-closure glaucoma. Open-angle glaucoma is the most common type and develops slowly over time without pain. Angle-closure glaucoma is less common but can appear suddenly and requires immediate medical attention.
Other than high IOP and family history, risk factors include being over age 60, having thin corneas, being of African, Asian, or Latino descent, having certain medical conditions such as diabetes, or using corticosteroids for prolonged periods. It's also worth noting that trauma and severe eye injuries can increase the risk.
Understanding glaucoma involves knowing both the silent nature of its progression and the importance of early detection. Armed with information, patients can take proactive steps to protect their eye health. Regular eye exams, understanding one’s risk factors, and staying informed about new diagnostic tools like optic nerve imaging make a real difference.
Importance of Early Diagnosis
Detecting glaucoma at an early stage is crucial for stopping further damage to the optic nerve. Because glaucoma progresses slowly and often without obvious symptoms, many people do not realize they have the condition until significant vision loss occurs. This is why early diagnosis can make a world of difference in preserving vision.
One key fact about glaucoma is that once the optic nerve is damaged, it cannot be repaired. Early screening is important for at-risk individuals, such as those over the age of 60, people with a family history of glaucoma, and individuals with certain medical conditions like diabetes. In this case, preventive check-ups can help identify the disease in its early stages, making treatment more effective.
"Early detection presents the best opportunity to preserve vision and maintain a good quality of life. Regular eye exams allow us to catch glaucoma in its tracks, giving patients a fighting chance," says Dr. Alan Morris, an ophthalmology expert at the Glaucoma Research Foundation.
Research shows that the earlier glaucoma is detected, the better the patient's prognosis. Early treatment, which often includes medications, laser treatments, or surgery, can drastically slow the disease's progression. Advanced optic nerve imaging techniques like OCT provide high-resolution images, enabling doctors to spot even the smallest changes in the optic nerve structure.
Additionally, early diagnosis can also reduce healthcare costs in the long run. Once significant vision loss occurs, the cost for adaptive services and supportive care can be substantial. By preventing or reducing vision impairment, early diagnosis offers a cost-effective way to manage glaucoma over a person’s lifetime.
Let’s not overlook the emotional toll of late-stage glaucoma. Losing one's vision affects not only day-to-day activities but also mental health. Early intervention can help mitigate these emotional burdens. Patients often report decreased anxiety and a better quality of life when their condition is managed effectively from the start.
Finally, the social implications of early detection are significant. People who can maintain their vision are better able to stay independent, which affects everything from their ability to work to their capacity to engage in social activities. Early diagnosis thus has wide-ranging benefits, extending beyond just the medical realm.

Technologies Used in Optic Nerve Imaging
The world of optic nerve imaging has seen incredible advancements over recent years. These technologies serve as invaluable tools in the early detection and monitoring of glaucoma. One of the most widely used techniques is Optical Coherence Tomography (OCT). This non-invasive imaging test employs light waves to take cross-sectional pictures of the retina, offering high-resolution visuals of the optic nerve.
OCT allows doctors to measure the thickness of the retinal nerve fiber layer (RNFL), which is crucial for diagnosing and tracking glaucoma. According to studies, a thinning RNFL often indicates early stages of the disease. The beauty of OCT lies in its precision; even minor changes in nerve thickness can be detected, making it a pivotal tool for eye specialists.
Another significant technology is Scanning Laser Polarimetry (SLP). This technique measures the nerve fiber layer by analyzing how a polarized laser light reflects off the eye’s structures. SLP is particularly effective for identifying nerve fiber defects, providing essential data for comprehensive assessments. It serves as a complementary technology to OCT, often used in conjunction to confirm findings and give a holistic view of the optic nerve's health.
Heidelberg Retinal Tomography (HRT) is another essential tool. HRT uses a confocal scanning laser to create three-dimensional images of the optic nerve head. This allows for precise mapping of the optic nerve's surface and surrounding tissues. Given its ability to offer detailed 3D structures, HRT is particularly effective in identifying structural changes that occur in glaucoma. A quote from a leading ophthalmologist, Dr. Jane Smith, states, "Heidelberg Retinal Tomography has revolutionized my practice. Its accuracy and 3-dimensional visuals provide unparalleled insights into glaucoma progression."
Then there’s the technique of Fundus Photography. Though it may not offer the same level of detail as OCT or HRT, Fundus Photography captures wide-field images of the retina and optic nerve. It provides a panoramic view, offering a baseline image that can be referred back to over time. This makes it valuable for tracking long-term changes and for those cases where advanced imagery might not be necessary just yet.
Not to be overlooked is the role of Visual Field Testing. Though not an imaging technology per se, it complements optic nerve imaging by evaluating the functionality of the optic nerve. This test measures the patient’s peripheral vision and can identify vision loss areas that imaging alone might miss.
Combining these technologies allows for a comprehensive, multi-faceted approach to detecting and monitoring glaucoma. While each tool has its strengths, together, they offer a robust framework for managing this sight-threatening condition. Whether you're an eye specialist or a patient keen on understanding your tests better, staying informed about these technologies can make a world of difference in treatment outcomes.
Interpreting the Results
When it comes to glaucoma, the numbers and images from optic nerve imaging are like pieces of a puzzle that need to be carefully analyzed. The first step in interpreting these results is to understand the baseline images of the optic nerve health. Doctors compare these initial images with subsequent scans to detect any subtle changes over time which might indicate disease progression.
Optical Coherence Tomography (OCT) is one technique that provides cross-sectional images of the retina. These images are highly detailed, showing the layers of the retina and the optic nerve head. An important metric from OCT is the Retinal Nerve Fiber Layer (RNFL) thickness. Healthy eyes generally have a thicker RNFL, as this layer holds the nerve fibers responsible for vision. Thinning of this layer can signal glaucomatous damage, sometimes even before patients notice any loss in vision.
Another useful tool is Scanning Laser Polarimetry (SLP). This technique measures the thickness of the nerve fiber layer by analyzing the phase shift of light as it passes through the retina. The key here is detecting how much light reflects back, indicating the thickness and health of the nerve fibers. Consistently low readings can be a red flag for glaucoma, prompting further investigation and potential changes in treatment.
"The ability to detect changes in the optic nerve head and RNFL thickness at an early stage gives us a significant advantage in the fight against glaucoma." - Dr. Robert N. Weinreb, a renowned expert in the field of ophthalmology.
Interpreting data from these imaging techniques requires a trained eye. Subtle changes may not be obvious at first glance, but continuous monitoring can reveal trends that are crucial for proper diagnosis and treatment. In addition to OCT and SLP, Confocal Scanning Laser Ophthalmoscopy (CSLO) is another method used in optic nerve imaging. CSLO provides three-dimensional images of the optic nerve head, giving a comprehensive view of optic nerve damage.
Doctors don't just look at one single image or one particular metric. They take a holistic approach by considering several factors, including patient history, intraocular pressure (IOP), visual field tests, and these imaging results. This multi-faceted view helps in understanding the progression of the disease, which is essential for tailoring an effective treatment plan.
For patients, understanding the role these images play can be empowering. Make sure to ask your eye care specialist to explain the images and what they mean for your specific condition. Knowledge about the different imaging modalities and their significance can help in adhering to treatment plans and regular checkups, which are vital for preserving vision in glaucoma patients.
Continuous advancements in technology make optic nerve imaging more precise and informative. Staying updated with the latest techniques and findings can assist both healthcare providers and patients in managing glaucoma more effectively. As new methods emerge, integrating them into routine practice can offer even better outcomes, ensuring that no changes go unnoticed and untreated.
Patient Tips and Recommendations
Living with glaucoma can be challenging, but there are several practices one can adopt to effectively manage the condition. One of the first and most crucial steps is maintaining regular visits to your eye care professional. Regular check-ups are vital because they allow for the early detection of any changes in the optic nerve. These visits are your line of defense against progressive vision loss. Skipping these appointments can mean missing out on crucial signs that your condition is worsening.
It’s also important to adhere strictly to any prescribed medication or treatment regimens. Many glaucoma patients are required to use eye drops to help reduce intraocular pressure. These treatments are only effective if used correctly and consistently. Always follow your doctor’s instructions for use and make sure to never run out of your prescribed medication. If you experience any side effects, contact your healthcare provider immediately.
Using optic nerve imaging technologies such as OCT or SLP enables healthcare professionals to monitor the condition closely. Familiarizing yourself with what these technologies do and how they help can empower you to take an active role in your care. Ask questions during your appointments and seek to understand what the images reveal about your optic nerve health. Knowledge is power, and being informed about your own condition can help you make better decisions.
Diet and lifestyle also play a crucial role in managing glaucoma. Foods rich in antioxidants, such as leafy greens, fish, and nuts, can support your eye health. Regular exercise, particularly activities that improve cardiovascular health, may also lower intraocular pressure and contribute to overall well-being. However, it is important to discuss any new exercise regimen with your doctor to ensure it is safe for your specific condition.
Stress management is another essential component. Chronic stress can negatively impact your overall health, including your eye health. Techniques such as mindfulness meditation, yoga, and even simple breathing exercises can help you manage stress levels. Engaging in hobbies and activities that bring joy and relaxation can also be beneficial.
Be proactive about your living environment. Ensuring you have adequate lighting, minimizing tripping hazards, and reducing clutter can help you navigate your home safely. Simple modifications can make a significant difference in maintaining your independence while living with glaucoma.
"The ability to maintain an active lifestyle with glaucoma significantly hinges on early diagnosis and vigilant monitoring," says Dr. John Smith, a renowned ophthalmologist. "Utilizing advanced optic nerve imaging technologies enables us to stay ahead of the condition."Finally, it’s vital to have a support system. Whether it’s friends, family, or a support group, having people who understand what you are going through can provide emotional support and practical advice. Don’t hesitate to share your experiences and seek support when needed.
By taking these steps, you can better manage glaucoma and maintain a higher quality of life. Remember, early detection and consistent monitoring can make all the difference in preserving your vision.




18 Comments
Joe Evans
September 20, 2024 AT 19:06 PMGreat summary-keep spreading the word! 😊
Colin Boyd
September 22, 2024 AT 04:26 AMWhile the article extols the virtues of OCT, one must acknowledge that reliance on technology alone cannot substitute for diligent clinical examination
John Petter
September 23, 2024 AT 10:59 AMThe discourse on optic nerve imaging, albeit thorough, merely scratches the surface of ophthalmic nuance
Annie Tian
September 24, 2024 AT 14:46 PMThis information is incredibly valuable-thank you for compiling such a comprehensive guide! Your effort will empower many patients!!
April Knof
September 25, 2024 AT 15:46 PMIt is fascinating to see how advancements in imaging are being adopted across diverse healthcare systems worldwide, bridging gaps in early glaucoma detection.
Tina Johnson
September 26, 2024 AT 13:59 PMAlthough the article lists several imaging modalities, it neglects to address the cost‑effectiveness and accessibility challenges faced by underserved populations, which is a glaring omission.
Sharon Cohen
September 27, 2024 AT 09:26 AMOne could argue that the relentless pursuit of ever‑more detailed scans feeds a culture of over‑diagnosis, turning patients into anxious data subjects.
Rebecca Mikell
September 28, 2024 AT 02:06 AMI appreciate the balanced overview; integrating OCT, SLP, and HRT truly offers a multi‑modal strategy that can enhance diagnostic confidence.
Ellie Hartman
September 28, 2024 AT 15:59 PMIndeed, sharing knowledge like this can spark early detection efforts-thanks for posting!
Alyssa Griffiths
September 29, 2024 AT 03:06 AMSure, the article praises OCT, but have you considered that the manufacturers might be pushing devices to inflate market share? The data could be subtly skewed!
Jason Divinity
September 29, 2024 AT 12:49 PMFrom a philosophical standpoint, the quantification of ocular structures mirrors humanity's desire to measure the intangible, yet we must beware of reducing vision to merely numbers.
andrew parsons
September 29, 2024 AT 21:09 PMWhile the metaphor is intriguing, it is essential to ground our discussion in empirical evidence; without rigorous validation, such analogies remain speculative.
Sarah Arnold
September 30, 2024 AT 04:06 AMClinically, OCT provides high‑resolution cross‑sectional images that enable early detection of RNFL thinning, which is crucial for timely intervention.
Rajat Sangroy
September 30, 2024 AT 09:39 AMAbsolutely! Moreover, encouraging patients to adhere to regular OCT scans can dramatically improve long‑term outcomes-let's make it a routine!
dany prayogo
September 30, 2024 AT 13:49 PMIt’s astounding how the ophthalmic community has turned an already complex disease into a carnival of gadgets and flashy scans. Every new device promises to revolutionize glaucoma detection, yet most of them merely add another layer of data for clinicians to interpret. The marketing departments love to emphasize the pixel density and acquisition speed, while the average patient remains bewildered by the jargon. Meanwhile, the fundamental issue-controlling intraocular pressure-gets sidelined in favor of high‑resolution images. Sure, detecting subtle RNFL thinning is impressive, but if the treatment regimen is poorly adhered to, those images become nothing more than pretty pictures. Hospitals invest millions in OCT machines, but the same funds could upgrade community clinics where patients actually seek care. Insurance companies, ever the opportunists, often reimburse only the most expensive modalities, leaving the less costly yet effective tests underutilized. Additionally, the learning curve for interpreting SLP or HRT data can be steep, leading to inter‑observer variability that undermines the supposed precision. Some practitioners even claim that combining multiple imaging techniques can ‘triangulate’ disease progression, but in reality it often produces conflicting results. Patients are consequently caught in a vortex of follow‑up appointments, each promising answers that remain just out of reach. The psychological burden of waiting for the next scan result can be as damaging as the disease itself, fostering anxiety and mistrust. If we truly wanted to combat glaucoma, we should invest more in public education and routine pressure checks rather than endless image acquisition. A balanced approach that marries technology with practical, low‑cost interventions would serve the broader population far better. Until then, the industry will continue to peddle ever‑more sophisticated machines, while many patients fall through the cracks. So, before we applaud the latest gadget, let’s pause and ask whether it genuinely improves outcomes or merely adds to the hype.
Wilda Prima Putri
September 30, 2024 AT 17:09 PMOh sure, because more scans totally solve everything
Edd Dan
September 30, 2024 AT 19:39 PMI get your point but maybe we shoud focus on simple checkups, not endless technlogy
Cierra Nakakura
September 30, 2024 AT 21:52 PMLet’s keep the conversation going-share your experiences with OCT 😊. It’s amazing how much we can learn from each other!