Chronic pain isn’t just a physical sensation-it’s a full-body experience that rewires how you think, feel, and move. If you’ve been living with pain for months or years, you’ve probably tried medications, physical therapy, injections, or even surgery. But what if the key to feeling better isn’t just fixing the injury, but changing how your mind responds to it? That’s where CBT for chronic pain comes in.
What Is CBT for Chronic Pain?
Cognitive Behavioral Therapy for Chronic Pain (CBT-CP) isn’t about pretending your pain isn’t real. It’s about understanding how your thoughts, emotions, and behaviors shape your experience of pain. Developed in the 1970s by pain psychologists like Dennis Turk and Robert Kerns, CBT-CP is built on one core idea: pain isn’t just a signal from your nerves-it’s filtered through your beliefs, fears, and habits.For example, if you believe “This pain means I’m getting worse,” you might stop moving altogether. That inactivity leads to stiffness, weakness, and more pain-a cycle that keeps going. CBT-CP breaks that cycle by teaching you how to recognize and change those automatic thoughts.
It’s not talk therapy in the traditional sense. There’s no lying on a couch recounting childhood trauma. Instead, it’s structured, practical, and skill-based. You learn tools you can use every day-like how to pace your activities, challenge catastrophic thinking, and relax your nervous system.
How CBT-CP Works: The Core Tools
Most CBT-CP programs run for 8 to 16 weekly sessions, each lasting about an hour. Whether you do it one-on-one with a therapist or in a group, the structure is similar. Here’s what you’ll actually do:- Pain neuroscience education: You learn how the nervous system works in chronic pain-not just damage, but sensitivity. This helps reduce fear. Many people feel relieved when they realize their pain isn’t a sign of ongoing damage.
- Activity pacing: Instead of pushing through pain until you crash (the “boom-bust” cycle), you learn to spread activities evenly. If you can walk 10 minutes today, you don’t wait until you feel 100% to do 20. You do 10, rest, and do another 10 later.
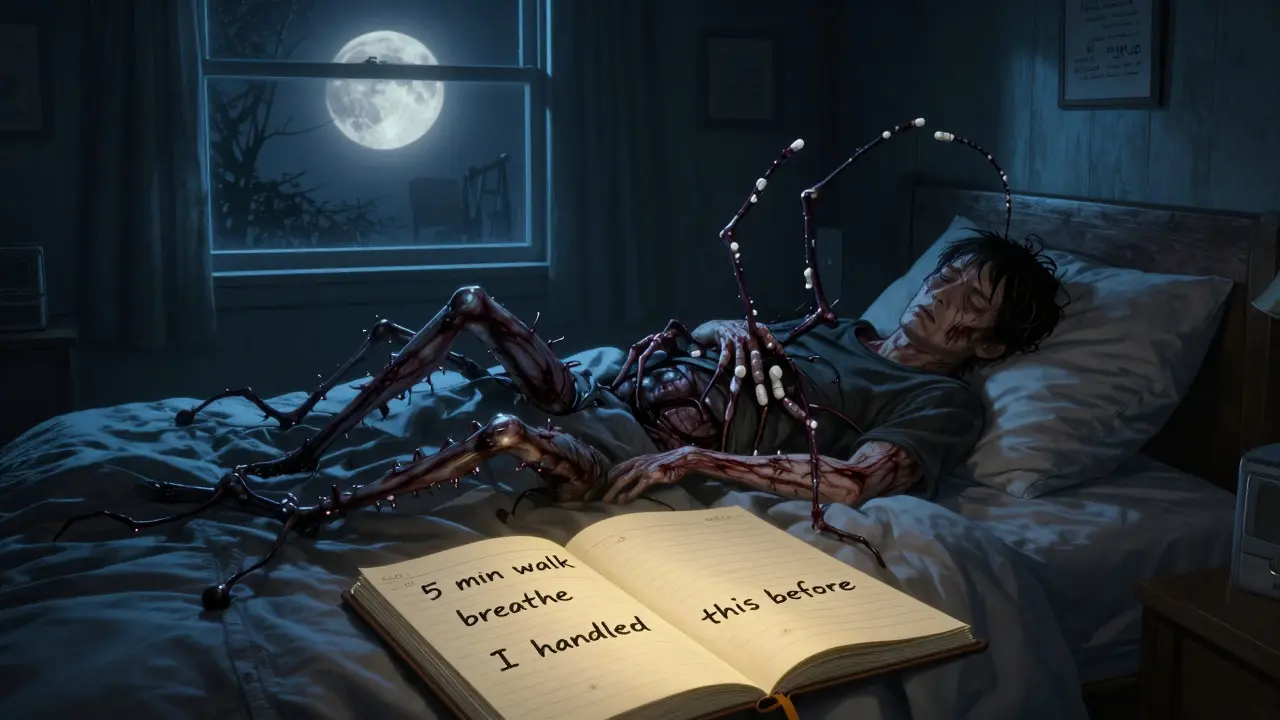
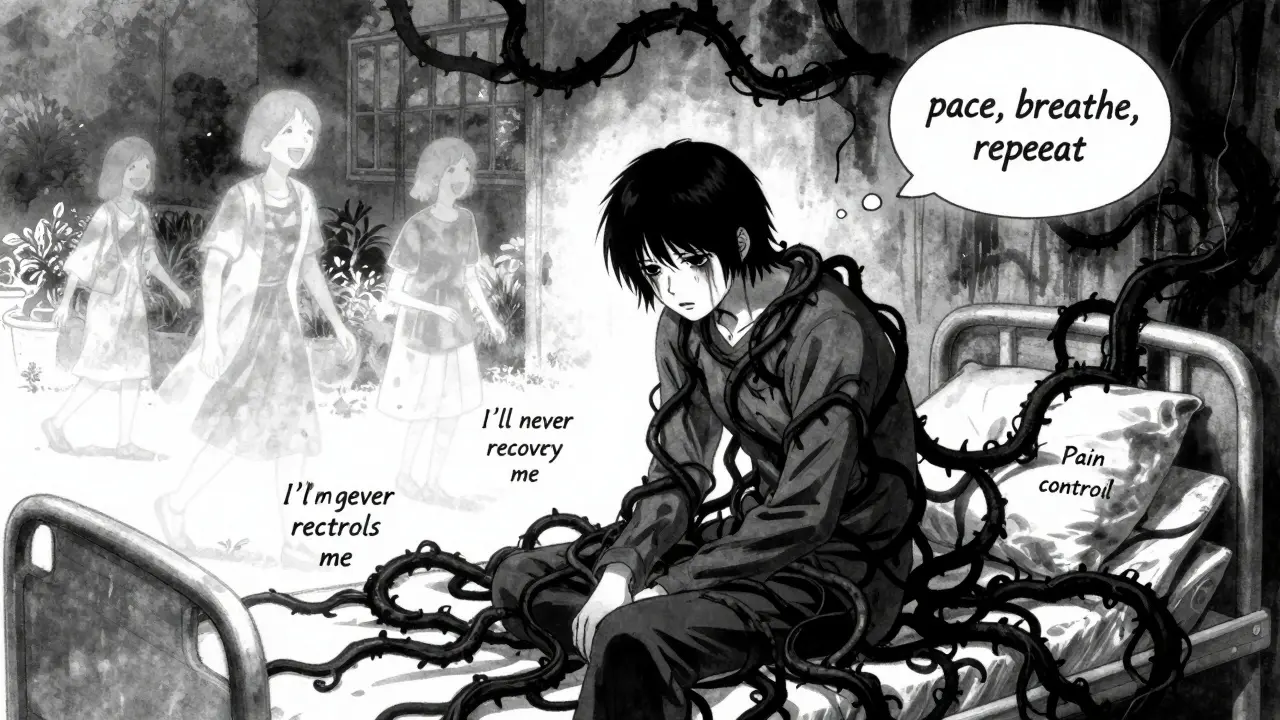
- Cognitive restructuring: You identify thoughts like “I’ll never get better” or “This pain controls my life” and replace them with more balanced ones: “I’m having a tough day, but I’ve handled this before.”
- Relaxation techniques: Deep breathing, progressive muscle relaxation, and mindfulness help calm your nervous system. Chronic pain keeps your body in fight-or-flight mode. These tools turn that down.
- Behavioral activation: When pain steals your motivation, you slowly rebuild meaningful activities-even small ones like gardening, calling a friend, or reading a book. It’s not about being pain-free; it’s about living again.
These aren’t abstract ideas. They’re skills you practice daily, like learning to play an instrument. The more you use them, the more automatic they become.
What Does the Research Say?
A 2023 review of 13 studies involving over 1,600 people found CBT-CP is the most studied psychological treatment for chronic pain-and it works. But not in the way most people expect.It doesn’t always make pain go away. In fact, only about 25% of studies showed a significant drop in pain intensity. That’s not because it’s ineffective-it’s because pain reduction isn’t the main goal.
What CBT-CP delivers consistently:
- Reduced depression: In 6 out of 8 studies, participants saw big drops in depressive symptoms.
- Lower anxiety: 5 out of 6 studies showed clear improvement.
- Better function: People reported being able to do more daily tasks-dressing, cooking, walking-without feeling overwhelmed.
- Less opioid use: In the 2024 STAMP trial, 36% of people in CBT-CP cut back on opioids. Only 17% did in the usual care group.
One study showed patients who completed at least 80% of sessions were 2.3 times more likely to report meaningful improvement. Consistency matters.
CBT-CP vs. Other Treatments
People often ask: “Is CBT better than physical therapy? Or mindfulness? Or medication?” The answer isn’t simple.Compared to physical therapy alone, CBT-CP doesn’t improve physical function more-but it does a much better job at improving mood and reducing fear of movement. Combine the two, and outcomes jump. One study found patients who got CBT-CP and physical therapy improved 40% more than those who got CBT alone.
Compared to mindfulness-based therapy (MBT), a 2024 JAMA study found no difference in pain or function after 26 weeks. Both were far better than standard care. So if you prefer meditation over thought journals, MBT is just as valid.
Compared to opioids? CBT-CP has no risk of addiction, overdose, or constipation. It doesn’t numb your body-it helps you reclaim your life. That’s why the VA and major pain societies now recommend it as a first-line treatment.

Who Benefits Most?
CBT-CP works best for people with:- Chronic low back pain
- Fibromyalgia
- Arthritis
- Chronic headaches or migraines
- Pain with depression, anxiety, or sleep problems
It’s less effective for pure nerve pain (like diabetic neuropathy) where the damage is more direct. But even then, it can help with the emotional toll.
Women make up 65% of CBT-CP patients. Why? Research suggests they’re more likely to seek psychological help and report higher levels of pain-related distress. But men benefit just as much-if they can get past the idea that “talking about pain is weak.”
College-educated patients use it more often, but that’s not because it’s harder to understand. It’s because they’re more likely to have access to specialists and insurance coverage.
Real People, Real Results
In the STAMP trial, one participant said: “Learning to pace my activities prevented my boom-bust cycles.” Another: “I stopped waiting for the pain to go away before I lived again.”On Reddit’s r/ChronicPain, people say things like:
- “I used to cancel plans every weekend. Now I go out-even if I’m sore.”
- “I cut my oxycodone in half after 6 weeks of CBT.”
- “I didn’t realize my fear of pain was making it worse.”
But it’s not magic. Some people say: “It felt like they were blaming me for my pain.” Others say: “It didn’t help during flare-ups.” That’s normal. CBT-CP doesn’t eliminate pain-it gives you tools to handle it better, even on bad days.
Barriers to Getting Started
The biggest problem? Access.Only 68% of U.S. commercial insurance plans cover enough CBT sessions. Medicare limits you to 10 per year-but most programs need 10 to 12 just to complete the basics. Private insurers vary wildly: UnitedHealthcare covers 12, Aetna covers 8.
Therapists trained in CBT-CP are rare. The VA trains its staff with 40 hours of specialized coursework and supervision. Most community clinics don’t have that.
And many patients are skeptical. “How can talking fix my back pain?” is a common reaction. That’s why successful programs use motivational interviewing-helping people explore their doubts instead of pushing them.
How to Find a CBT-CP Therapist
Start here:- Ask your pain specialist or primary care doctor for a referral. Many now have partnerships with psychologists.
- Check the American Psychological Association’s psychologist locator. Filter for “chronic pain” or “health psychology.”
- Look for therapists who use the VA’s CBT-CP protocol or have training from the International Association for the Study of Pain.
- Ask: “Do you use activity pacing and cognitive restructuring for chronic pain?” If they say no, keep looking.
If in-person therapy isn’t possible, digital options are growing fast. FDA-cleared apps like MyPainCoach and Chronic Pain Coach now offer structured CBT-CP modules. A 2021 study found video-based CBT worked just as well as in-person.
What to Expect in Your First Session
You won’t be asked to “think positive.” You’ll be asked to track your pain for a week: when it’s worse, what you were doing, what you thought, how you felt. That’s your baseline.Your therapist will explain the biopsychosocial model: pain = biology + thoughts + behavior. You’ll get a workbook. You’ll set one small goal: “Walk for 5 minutes every other day.” No pressure. No judgment.
The goal isn’t to be pain-free. It’s to be alive-even with pain.
Is CBT-CP Right for You?
Ask yourself:- Do I feel stuck in a cycle of pain → fear → inactivity → more pain?
- Have I tried medications or procedures but still feel limited?
- Am I tired of waiting for a miracle cure?
- Do I want tools I can use every day, not just when I’m in the clinic?
If you answered yes to any of these, CBT-CP could help.
It’s not a quick fix. But it’s one of the few treatments proven to change your life-not just your pain level.
Can CBT for chronic pain make my pain go away completely?
No, CBT-CP doesn’t eliminate pain. Its goal is to reduce how much pain controls your life. Many people still feel pain but report being able to work, sleep, and enjoy activities again. Studies show it improves mood, function, and quality of life more reliably than it reduces pain intensity.
How long does it take to see results from CBT for chronic pain?
Most people start noticing changes in mood and activity levels after 4 to 6 weeks. Improvements in sleep, anxiety, and daily function often show up before pain decreases. Full benefits typically take 8 to 12 sessions. Consistency is more important than speed.
Is CBT-CP covered by insurance?
Coverage varies. Medicare covers up to 10 sessions per year. Private insurers range from 8 to 12 sessions. Some plans require pre-authorization or limit you to in-network providers. The VA covers full CBT-CP programs for veterans. Always call your insurer and ask: “Do you cover Cognitive Behavioral Therapy for Chronic Pain under behavioral health benefits?”
Can I do CBT for chronic pain on my own?
You can use apps, books, or online programs, and many people benefit. But working with a trained therapist increases success by 30-50%. Therapists help you spot unhelpful thought patterns you might miss, adjust techniques to your needs, and keep you accountable. For best results, combine self-guided tools with at least a few sessions with a professional.
Does CBT-CP work for neuropathic pain?
It’s less effective for nerve pain like diabetic neuropathy or post-surgical nerve damage, where the physical cause is more direct. But it still helps with the emotional burden-fear, frustration, sleep loss-that often makes neuropathic pain feel worse. Many patients report better coping, even if the burning or tingling doesn’t disappear.
What if I don’t believe my pain is in my head?
That’s a common concern-and CBT-CP doesn’t claim your pain is “all in your head.” It’s real. The therapy works because your brain processes pain through emotions, memories, and beliefs. Think of it like this: a broken leg hurts more if you’re terrified it won’t heal. CBT-CP helps reduce that fear, not deny the injury. You’re not being told to “think happy thoughts.” You’re learning how your mind influences your experience of pain.





11 Comments
Betty Bomber
January 26, 2026 AT 19:28 PMBeen doing CBT for my fibro for 6 months now. Didn't expect it to help, but I actually sleep better and don't cancel plans anymore. My pain's still there, but it doesn't own me.
Sally Dalton
January 27, 2026 AT 07:38 AMOMG YES THIS. I used to think if i wasn't 100% i shouldn't move at all... then i'd crash for days. Pacing changed EVERYTHING. I walk 10 mins, sit, walk 10 more. Feels silly but it works. My husband says i'm less grumpy too lol.
Curtis Younker
January 28, 2026 AT 12:24 PMLet me tell you, this isn't some woo-woo mind-over-matter crap. I was skeptical too-thought it was just therapists telling people to ‘think positive’ so they’d stop complaining. But when I learned how my nervous system was stuck in overdrive like a car with the gas pedal welded down? That clicked. I started doing the breathing exercises before bed, tracked my thoughts when pain spiked, and honestly? I went from crying in the shower every morning to making coffee and watching the sunrise without wanting to die. It’s not magic. It’s like retraining your brain’s alarm system. And yeah, I still have bad days. But now I know it’s not a sign I’m failing-it’s just the system glitching. And I’ve got tools to handle it. If you’re on the fence? Just try one session. What’s the worst that happens? You learn something new about your own body. And that’s worth it.
Shawn Raja
January 30, 2026 AT 01:09 AMOf course talking fixes pain. Just like how yelling at your Wi-Fi router makes the internet faster. /s
But seriously-this works because pain isn’t just a signal. It’s a story your brain keeps telling itself. And if you keep rewinding the same traumatic episode over and over, of course it loops. CBT doesn’t erase the scar-it stops you from picking at it. Also, I’m shocked anyone still thinks opioids are the answer. We turned a medical crisis into a marketing campaign and now we’re paying the price in overdoses and broken families. Meanwhile, people are learning to live again. Not perfect. Not pain-free. But alive. That’s the real win.
Ryan W
January 30, 2026 AT 22:48 PMAnother liberal pseudoscience racket disguised as medicine. Pain is biological. If your spine is degenerated, your nerves are inflamed, or your discs are herniated-no amount of ‘thought restructuring’ will undo structural damage. This is just the medical establishment’s way of avoiding real diagnostics and pushing cheap, ineffective therapy because insurance won’t pay for MRIs anymore. If you’re not getting imaging, labs, or surgical consults before CBT, you’re being gaslit. Real pain needs real solutions-not affirmations.
Henry Jenkins
January 31, 2026 AT 18:09 PMI appreciate the data here, especially the 2.3x improvement rate for consistent participants. But I wonder-how many people drop out before 8 sessions? The barrier isn’t just access, it’s motivation. Chronic pain drains willpower. If you’re exhausted, depressed, and in constant discomfort, asking someone to journal their thoughts and do 5-minute walks feels like adding another chore to a broken system. Maybe we need more ‘low-effort entry points’-like automated app nudges or peer-led check-ins. CBT’s great, but it assumes you’ve got the mental bandwidth to engage with it. What about the people who can barely get out of bed? How do we reach them without making them feel guilty for not ‘trying hard enough’?
Napoleon Huere
February 2, 2026 AT 01:05 AMThere’s a deeper truth here that nobody says out loud: chronic pain isn’t just a condition-it’s a social contract. Society expects you to be productive, mobile, happy. When you can’t, you become invisible. Or worse, a burden. CBT doesn’t fix your spine, but it lets you reclaim your dignity. You stop apologizing for existing in pain. You stop pretending you’re ‘fine.’ You stop letting others define your worth by your output. That’s revolutionary. In a world that equates value with performance, choosing to live fully despite pain? That’s not therapy. That’s resistance.
Shweta Deshpande
February 3, 2026 AT 04:35 AMI’m from India and my mom has arthritis-she refused to try anything but Ayurveda until last year. I showed her this stuff, translated the pacing part into Hindi, and she started doing it with her daily chores. Now she cooks, gardens, even plays with her grandkids without collapsing. She says, ‘I thought my body was broken. Turns out, my mind was the lock.’ I cried when she told me that. This isn’t just Western medicine-it’s human. And it works anywhere, if you let it.
Aishah Bango
February 3, 2026 AT 18:12 PMWhy are we praising this like it’s some moral victory? People are being told their pain is ‘in their head’ and then congratulated for ‘managing’ it instead of curing it. This is victim-blaming dressed up as empowerment. If your body is failing, fix the body. Don’t make people feel guilty for not being ‘positive’ enough. This isn’t healing-it’s surrender.
Jessica Knuteson
February 4, 2026 AT 01:53 AMCBT works because it’s cheaper than surgery and doesn’t require FDA approval. The system doesn’t care if you’re in pain. It cares if you’re functional. So they give you tools to pretend you’re not suffering. That’s not treatment. That’s management. And management is just capitalism’s way of making suffering bearable enough to keep you working.
Robin Van Emous
February 6, 2026 AT 00:09 AMJust wanted to say thank you for writing this so clearly. I’m 58, had back surgery 3 years ago, and still hurt. My therapist used this exact framework-pacing, cognitive restructuring, the whole thing. I didn’t believe it at first. But I kept doing the little things. Now I garden. I walk my dog. I read novels again. I still have pain. But I don’t hate my life anymore. And that’s worth more than any pill.