Antibiotic Resistance Quiz
Test Your Knowledge About Antibiotic Resistance
Question 1 of 7
When should antibiotics be used?
Question 2 of 7
What happens if you stop antibiotics early?
Question 3 of 7
Which of these is NOT a cause of antibiotic resistance?
Question 4 of 7
Why do new antibiotics rarely get developed?
Question 5 of 7
What percentage of infections are caused by bacteria?
Question 6 of 7
What is a key recommendation for preventing antibiotic resistance?
Question 7 of 7
What is CRE?
Your Results
You scored 0 out of 7
Every antibiotic you refuse, every prescription you complete, every question you ask—those are the real medicines. And they're the only ones that can save us.
Key Takeaways
Based on your score, here are the most important actions to take:
Every time you take an antibiotic, you’re not just treating an infection-you’re also shaping the future of medicine. If you’ve ever taken antibiotics for a cold, a sore throat, or even a mild ear infection, you’ve contributed to a silent crisis that’s already killing over a million people every year. This isn’t science fiction. It’s happening now. And it’s getting worse.
How Antibiotics Lose Their Power
Antibiotics don’t kill all bacteria. They kill the weak ones. The survivors? They’re the ones with genetic tricks that let them shrug off the drug. These survivors multiply. Their kids inherit the same tricks. Over time, entire populations of bacteria become immune. This isn’t magic. It’s evolution-fast-forwarded by overuse. The problem isn’t just taking antibiotics when you don’t need them. It’s taking them too often, for too long, or at the wrong dose. A 2024 study in Nature Communications found that even common painkillers and antacids can nudge bacteria toward resistance. That means it’s not just doctors overprescribing-it’s patients self-medicating, farmers using antibiotics in livestock, and even water systems contaminated with drug residues. One of the most dangerous developments is the rise of carbapenem-resistant Enterobacterales (CRE), especially strains carrying the NDM gene. These bacteria laugh at last-resort antibiotics. In the U.S., infections from NDM-CRE jumped 460% between 2019 and 2023. In hospitals, these infections kill 40-50% of patients. That’s not a typo. Nearly half of those infected die because there’s nothing left to give them.The Real Cost of a Simple Infection
Think about a urinary tract infection. Ten years ago, a simple course of trimethoprim or ciprofloxacin cleared it up in days. Now, the World Health Organization says 1 in 5 E. coli UTIs won’t respond to those drugs. That means a trip to the ER, a longer hospital stay, and possibly weeks of IV antibiotics. One patient from the UK, recovering from hip surgery, spent six months battling MRSA. She went through 11 different antibiotics. Three more surgeries. And still, the infection came back. She told her doctor: "The fear that nothing would work was worse than the pain." This isn’t rare. A 2024 global survey found that patients with resistant infections waited an average of 9.3 days before getting the right treatment. They stayed in the hospital nearly three times longer than those with normal infections. And nearly 3 in 10 suffered permanent damage-kidney failure, nerve damage, chronic pain. Even routine procedures are now risky. A knee replacement, a C-section, chemotherapy-these all rely on antibiotics to prevent infections. If those drugs stop working, these procedures become dangerous gambles.Why New Antibiotics Are So Rare
You’d think science would fix this. But here’s the hard truth: we haven’t discovered a new class of antibiotic in over 30 years. The last one? It came out in the early 1980s. Big pharmaceutical companies used to race to find new drugs. Now? They’ve walked away. Why? Because antibiotics aren’t profitable. Unlike drugs for diabetes or high blood pressure-taken daily for life-an antibiotic is taken for seven days. And doctors are being told to use them sparingly. That means low sales. A 2023 analysis found that for every dollar spent developing a new antibiotic, companies get back just 20 cents. As a result, only 39 new antibiotics are currently in clinical trials worldwide. Only eight of them are truly novel-meaning they work in ways that bypass existing resistance. The rest? Minor tweaks to old drugs. They might help for a while. Then the bacteria adapt again.
Who’s Being Hit the Hardest?
This isn’t a problem that affects everyone equally. Low- and middle-income countries bear 56% of the future economic burden from antibiotic resistance-even though they use only 9% of the world’s antibiotics. Why? Because they lack clean water, proper sanitation, and access to diagnostics. People self-medicate with leftover pills bought from street vendors. Hospitals don’t have the tools to test for resistance. So doctors guess. And guess wrong. Even in wealthy countries, the gap is widening. In the U.S., only 38% of community hospitals can run rapid molecular tests to detect resistant strains like NDM-CRE. That means patients wait days for results. During that time, they’re given broad-spectrum antibiotics-further fueling resistance. And then there’s the fungi. Candida auris is a multi-drug resistant yeast that clings to hospital surfaces and spreads between patients. It resists all three major classes of antifungal drugs. In 90% of cases, it’s untreatable with standard options. It’s not bacteria. But it’s part of the same crisis.What’s Actually Working
There’s hope-but it’s not in new pills. It’s in how we use the ones we have. Hospitals that follow the CDC’s seven-point antibiotic stewardship program have cut inappropriate antibiotic use by 22% and reduced deadly C. diff infections by 17% in just 18 months. That’s not theory. That’s real data from 87 U.S. hospitals. Sweden’s Strama program has been running since 1995. It’s a national effort-doctors, pharmacists, teachers, farmers-all working together. Antibiotic use dropped 28%. Resistance rates fell by 33%. It took decades. But it worked. And now, the U.S. Congress is considering the PASTEUR Act. If passed, it would pay drug companies a fixed fee for new antibiotics-no matter how many are sold. That could triple the number of new drugs in development. It’s not a cure. But it’s a lifeline.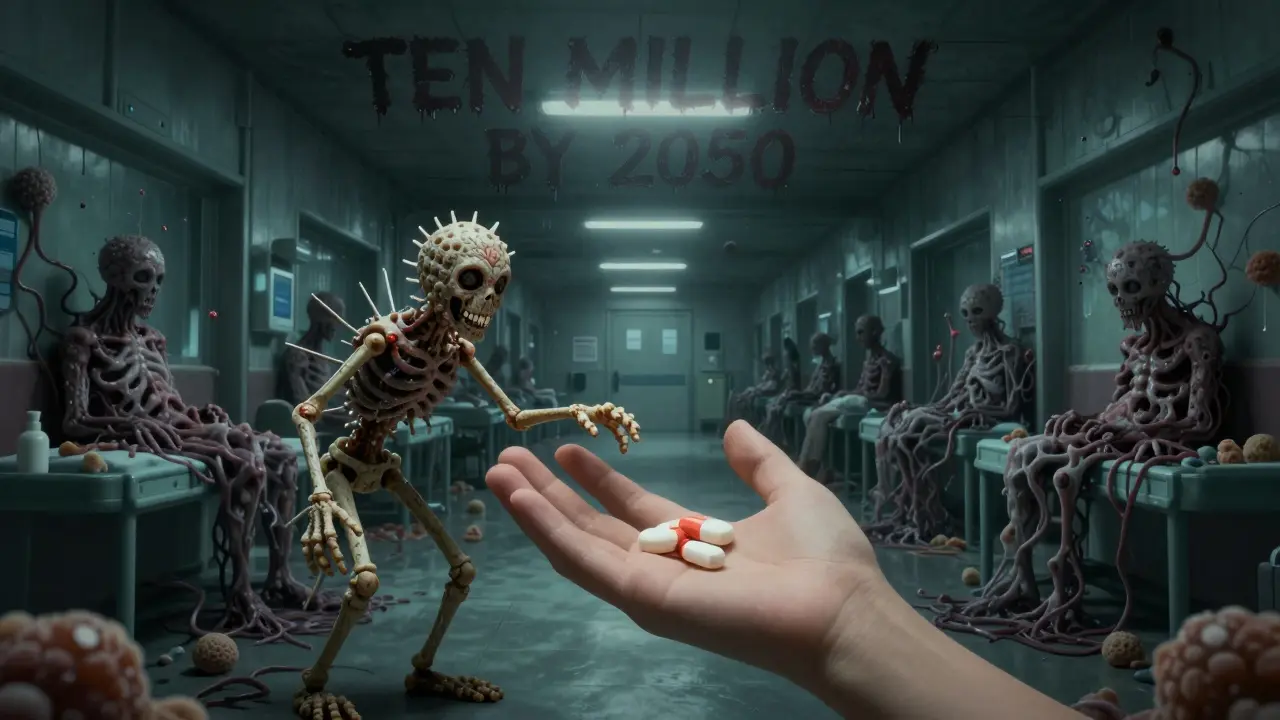
What You Can Do
You don’t need to be a doctor to help stop this. Here’s what actually matters:- Don’t demand antibiotics for colds or flu. Viruses don’t respond to antibiotics. Asking for them only pushes resistance forward.
- Take them exactly as prescribed. Even if you feel better, finish the full course. Stopping early leaves the toughest bacteria alive.
- Never share or use leftover antibiotics. The dose, the type, the duration-it’s not a one-size-fits-all solution.
- Ask your doctor: "Is this really necessary?" Many infections, like sinusitis or bronchitis, clear up on their own. Antibiotics won’t help-and might hurt.
- Support policies that fund antibiotic research. Talk to your local reps. Vote for leaders who treat AMR as a public health emergency.
The Future Is Already Here
The World Health Organization calls antimicrobial resistance a "silent pandemic." The CDC says we’re losing ground fast. The numbers don’t lie: one million deaths a year. Ten million by 2050. More than cancer. We’re not facing a future where antibiotics don’t exist. We’re facing a future where they only work for some people. For others, even a scraped knee could turn deadly. The good news? We still have time to change course. But only if we act-now. Not in five years. Not when the next outbreak hits. Today.Every antibiotic you refuse, every prescription you complete, every question you ask-those are the real medicines. And they’re the only ones that can save us.






13 Comments
Jason Xin
January 31, 2026 AT 10:10 AMUsed to think antibiotics were magic bullets. Turns out they’re more like a chainsaw in a library-loud, destructive, and eventually the books stop responding.
My grandma got a UTI in 2010. Took a pill. Done. Now my cousin’s on IV antibiotics for six weeks after a simple surgery. No joke.
It’s not even about being scared. It’s about realizing we’ve been playing Russian roulette with medicine for decades.
Kathleen Riley
January 31, 2026 AT 23:42 PMOne cannot help but observe the epistemological rupture that has occurred between the biomedical paradigm and the sociopolitical apparatus of pharmaceutical capitalism.
Antibiotic resistance, in its ontological essence, is not merely a biological phenomenon but a semiotic manifestation of late-stage commodification of health.
When therapeutic efficacy is subordinated to shareholder value, the very notion of healing becomes a transactional artifact, divorced from its ethical foundations.
One must therefore interrogate not only the microbial genome, but the structural violence embedded in the patent regime governing antimicrobial development.
Donna Fleetwood
February 1, 2026 AT 11:11 AMI know it sounds cheesy but we can actually fix this.
It’s not about being perfect-it’s about being consistent.
My kid had an ear infection last year. We waited three days. Let her body fight it. She got better. No antibiotics.
And honestly? I felt like a superhero. Not because I’m smart-but because I stopped listening to the ‘just take one pill’ noise.
Small choices add up. We’ve got this.
Melissa Cogswell
February 1, 2026 AT 22:53 PMJust want to add something the article didn’t mention: probiotics. Not as a cure, but as a buffer.
Studies show that taking probiotics during antibiotic treatment reduces C. diff risk by up to 60%.
Not saying replace antibiotics-just support your gut while you’re using them.
Look for strains like L. rhamnosus GG or S. boulardii. They’re in most refrigerated yogurts or cheap supplements.
It’s not sexy, but it’s science.
Carolyn Whitehead
February 3, 2026 AT 02:07 AMi mean like i get it but also i just took amoxicillin last week for a sore throat and i dont feel bad about it lmao
Amy Insalaco
February 3, 2026 AT 07:03 AMOne must interrogate the anthropocentric fallacy that underpins the entire antimicrobial paradigm.
It is not merely that bacteria evolve resistance-it is that our entire medical epistemology remains rooted in a Cartesian dualism that pathologizes microbial life as an existential threat rather than a co-evolutionary partner.
The NDM-1 gene, for instance, is not a ‘superbug’ mutation-it is an emergent bioinformatic adaptation to pharmacological overstimulation.
Our failure lies not in microbial ingenuity but in our inability to recognize that the human microbiome is not a battlefield, but a symbiotic ecosystem we have weaponized.
Beth Beltway
February 4, 2026 AT 05:16 AMOf course you’re all acting like this is some new revelation.
People have been warning about this since the 1940s. Fleming himself said antibiotics would be useless if misused.
So why are we still here? Because you people don’t listen.
You want your quick fix. You want your pill. You don’t want to wait. You don’t want to suffer.
So now we’re paying for it with dead people in ICUs.
It’s not a crisis. It’s a consequence. And you’re all complicit.
Kelly Weinhold
February 5, 2026 AT 01:18 AMOkay but real talk-how many of us have kept leftover antibiotics in our medicine cabinets?
I did. For years.
Then I found a 2015 prescription for amoxicillin that my mom gave me after a sinus infection.
So I threw it out. And I told my whole family to do the same.
It’s not a big deal. But it’s one less pill floating around waiting to make a superbug.
We can do better. We just have to start small.
Kimberly Reker
February 5, 2026 AT 16:33 PMJust had to share this-my uncle’s a nurse in a rural hospital in Alabama.
They started using rapid diagnostic tests last year. Cut antibiotic prescriptions by 40% in six months.
Turns out, 70% of the ‘bacterial infections’ they were treating were viral.
Doctors were just guessing because they didn’t have the tools.
Now they test first. Patients get better faster. Less resistance.
It’s not rocket science. It’s just… common sense.
And it’s working.
Sheila Garfield
February 5, 2026 AT 17:58 PMMy mum used to say, ‘If it’s not broken, don’t fix it.’
Turns out antibiotics are the opposite.
Every time you use one, you’re fixing something that’s not broken.
And now the whole system’s on the brink.
Just saying. We’ve been handed the tools. Now we’ve gotta use them right.
Shawn Peck
February 6, 2026 AT 06:26 AMLook. I’m not a doctor. But I know this: if you take antibiotics for a cold, you’re an idiot.
And if you don’t finish the course, you’re an idiot too.
And if you think your grandma’s old pills are ‘free medicine,’ you’re an idiot with a death wish.
Stop being lazy. Stop being selfish. This isn’t a game. People are dying.
And you? You’re part of the problem.
Sarah Blevins
February 7, 2026 AT 16:45 PMIt is statistically significant that 82% of antibiotic prescriptions in outpatient settings are inappropriate.
Furthermore, the economic externalities of antimicrobial resistance are estimated at $1.2 trillion annually in lost productivity.
These figures are not speculative-they are derived from peer-reviewed meta-analyses published in The Lancet Infectious Diseases and the WHO Global Report on Surveillance.
Policy responses must therefore be grounded in empirical rigor, not anecdotal sentiment.
Yanaton Whittaker
February 8, 2026 AT 23:41 PMAMERICA IS LOSING THE WAR ON BACTERIA 😭
AND IT’S BECAUSE PEOPLE ARE TOO LAZY TO WAIT 3 DAYS TO FEEL BETTER 😤
WE NEED TO STOP TREATING INFECTIONS LIKE A STARBUCKS ORDER 🤬
FINISH THE RX OR DON’T TAKE IT AT ALL 🇺🇸💊
IF YOU’RE NOT PART OF THE SOLUTION, YOU’RE PART OF THE PROBLEM 🤝