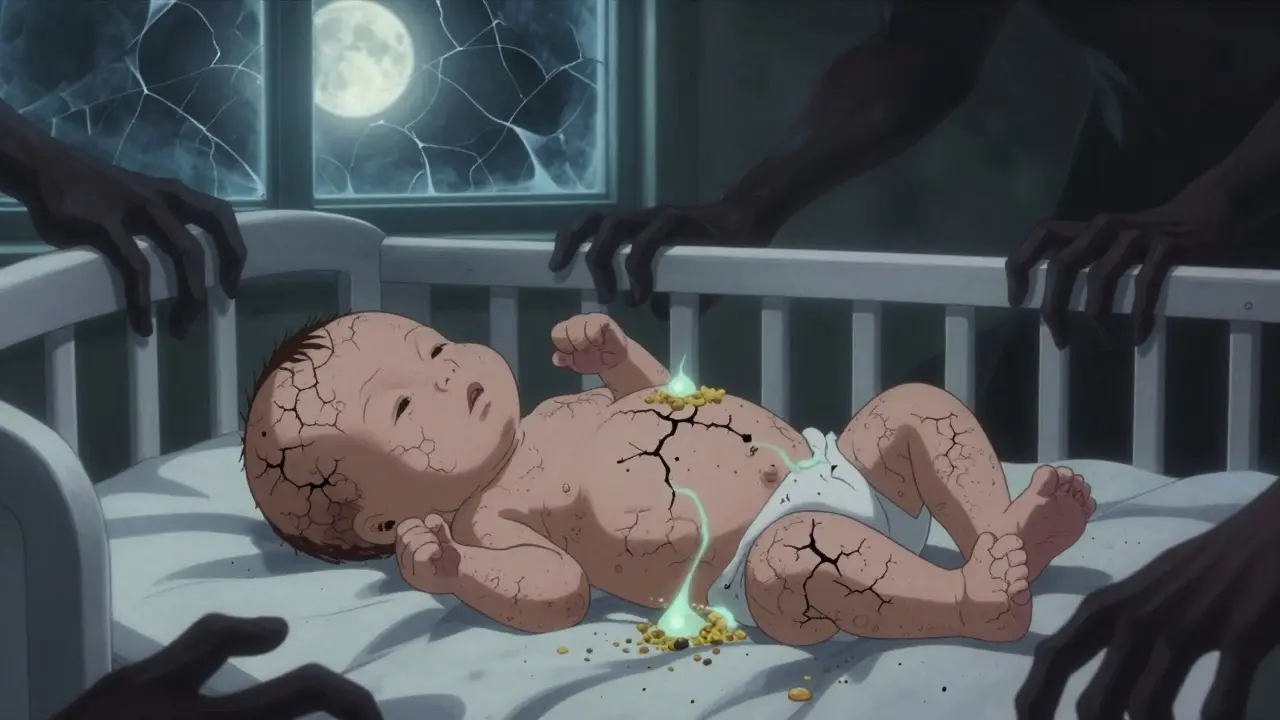
When a baby develops dry, itchy skin in the first few months of life, it’s easy to think it’s just a temporary rash. But for many, that patch of eczema isn’t just a skin problem-it’s the first sign of something bigger. This is the atopic march: a pattern where eczema often leads to food allergies, then asthma, and later allergic rhinitis. But here’s the twist: it doesn’t happen to everyone. In fact, most kids with eczema never develop asthma. The real story isn’t about inevitability-it’s about risk, timing, and what you can do to change the course.
What the Atopic March Really Means
The term "atopic march" was coined decades ago to describe how allergic diseases seem to show up one after another in children. It started with eczema, then food allergies, then asthma, and finally hay fever. It sounded simple: if your child has eczema, they’re on a path toward other allergies. But recent studies have turned that idea upside down.
A 2023 analysis of over 10,000 children found that only 3.1% followed the classic sequence. That’s not a trend-it’s an exception. Most kids with eczema don’t go on to develop asthma. And many kids with asthma never had eczema. So why does the pattern still matter?
The answer lies in the skin barrier. When the skin’s outer layer breaks down-especially in babies with a genetic mutation in the filaggrin gene-it doesn’t just get dry. It becomes a doorway. Allergens like peanut proteins, egg, and cow’s milk can slip through cracks in the skin, triggering the immune system to react. That reaction doesn’t just cause a rash. It trains the immune system to overreact later, even to things you breathe in.
That’s why researchers now talk about "atopic multimorbidity" instead of a linear march. It’s not a straight line. It’s a cluster. Eczema, food allergies, asthma, and rhinitis often show up together-not because one causes the other, but because they share the same root: a faulty skin barrier and an immune system that got confused early on.
Why Skin Barrier Breakdown Is the Starting Point
Think of your skin like a brick wall. The bricks are skin cells. The mortar is the proteins that hold them together. In kids with eczema, the mortar is weak. The most common flaw? A mutation in the filaggrin gene. This gene makes a protein that keeps the skin moist and protected. When it’s broken, the skin loses water, gets dry, cracks, and lets allergens in.
Studies show that babies born with visibly dry skin-even before a rash appears-are at higher risk. In one study, infants with dry skin at birth were three times more likely to develop eczema by three months. And once eczema sets in, the risk of food allergy jumps. The LEAP study proved this: high-risk infants with severe eczema who were given peanut protein orally before age 1 had an 86% lower chance of developing peanut allergy by age 5.
But here’s the catch: if that same peanut protein touched their cracked skin first? They were more likely to become allergic. This is the dual-allergen exposure hypothesis. Skin exposure = sensitization. Oral exposure = tolerance.
It’s not just filaggrin. Mutations in genes like SPINK5 and corneodesmosin also weaken the skin barrier. And genes that control immune signals-like TSLP and IL-33-amplify the response. When these genes go haywire, the immune system doesn’t just react to peanut. It starts reacting to dust mites, pollen, and pet dander. That’s why kids with eczema often end up with multiple allergies.
How Severe Eczema Changes the Game
Not all eczema is the same. Mild flares on the cheeks? Common. Thick, oozing patches on the arms and legs? That’s a red flag.
The MAS cohort study found that kids with severe eczema were 3 to 4 times more likely to develop multiple allergic conditions. The BAMSE study showed that severe eczema increased asthma risk by over 60% compared to mild cases. And among children with asthma, 74% to 81% also had allergic rhinitis-usually starting around age 3.
But here’s what most parents don’t realize: 80% of children with eczema develop sensitization to allergens-meaning their immune system recognizes them. But only a fraction ever develop symptoms. That’s the difference between a positive allergy test and a real allergic reaction. A child can test positive for egg and still eat it without a problem. The test doesn’t tell you if they’ll get sick. It just tells you their immune system noticed it.
This is why blanket warnings don’t work. You can’t tell every child with eczema to avoid eggs or dairy. But you can look for signs of severity: persistent itching, sleep disruption, skin infections, or eczema that doesn’t respond to basic moisturizers. That’s the group that needs attention.

What You Can Do: Skin Barrier Care That Works
If the skin barrier is the gateway, then repairing it is the first line of defense. And it’s not about creams alone-it’s about consistency, timing, and the right ingredients.
- Start early: Apply fragrance-free emollients (moisturizers) daily from birth-even if there’s no rash yet. The PreventADALL trial showed this reduced eczema incidence by 20-30% in high-risk infants.
- Use the right products: Look for creams with ceramides, cholesterol, and fatty acids. These are the building blocks of healthy skin. Avoid products with alcohol, fragrance, or essential oils.
- Apply after baths: Soak for 5-10 minutes in lukewarm water. Pat dry, then apply moisturizer within 3 minutes. This locks in moisture better than any product alone.
- Think beyond the skin: Gut health matters too. Research shows infants with reduced gut bacteria that produce butyrate are more likely to develop multiple allergies. While we don’t yet have a probiotic pill for this, breastfeeding and introducing diverse foods (like vegetables, legumes, and whole grains) after 6 months may help.
And yes-early introduction of allergens works. The LEAP study didn’t just prove peanut avoidance was wrong. It proved that feeding peanut protein to high-risk babies, under medical guidance, could prevent allergy. The same logic applies to egg, milk, and sesame. Don’t delay. Talk to your pediatrician about safe introduction, especially if your child has severe eczema.
What Doesn’t Work (And Why)
There’s a lot of noise out there. You’ve heard that organic diets, herbal creams, or strict elimination diets can prevent allergies. None of those have strong evidence.
Removing dairy from a breastfeeding mom’s diet? Doesn’t reduce eczema risk in most cases. Switching to hypoallergenic formula? Only helps if the baby has a confirmed cow’s milk protein allergy-not just eczema. Using expensive "allergy-preventing" creams with plant extracts? Often just expensive moisturizers with added irritants.
And don’t assume that if your child has eczema, they’ll definitely get asthma. Only about 25% do. That means 75% won’t. The goal isn’t to scare parents. It’s to focus on the ones who need help.
The key is not to treat every child the same. It’s to identify the ones with severe eczema, family history of asthma or allergies, and early skin barrier breakdown-and give them targeted support.

The New Approach: Precision, Not Prediction
Doctors are moving away from saying, "Your child has eczema, so they’ll get asthma." Instead, they’re asking: What’s the severity? What’s the family history? Are there filaggrin mutations? Is the skin barrier intact? Is the gut microbiome showing signs of imbalance?
Researchers are now building predictive tools using these factors. Some clinics already test for filaggrin mutations in infants with severe eczema. Others track skin hydration levels over time. The goal? To find the 25% who are truly at risk-and help them before it escalates.
This is precision medicine for allergies. It’s not about preventing all allergies. It’s about preventing the ones that matter most-the ones that lead to asthma, hospital visits, or lifelong food restrictions.
And the best part? You don’t need a genetic test to start. Daily moisturizing. Early, safe allergen introduction. Avoiding harsh soaps. These are simple, low-risk, high-reward actions.
Final Thoughts: It’s Not a March-It’s a Choice
The atopic march isn’t a fate. It’s a warning sign. Eczema isn’t just a rash. It’s your child’s body telling you something’s off with their skin-and maybe, their immune system. But you’re not powerless.
Every time you moisturize, you’re strengthening a barrier. Every time you introduce peanut or egg safely, you’re teaching the immune system to stay calm. Every time you avoid scented lotions and hot baths, you’re reducing triggers.
You can’t change genetics. But you can change how the skin behaves. And that’s enough to change the outcome.