Heart failure isn’t a single disease-it’s a condition where the heart can’t pump enough blood to meet your body’s needs. And while lifestyle changes matter, medications are what actually save lives and keep people out of the hospital. Four drug classes form the backbone of modern treatment: ACE inhibitors, ARNIs, beta blockers, and diuretics. Together, they don’t just manage symptoms-they change the course of the disease.
ACE Inhibitors: The First Line for Decades
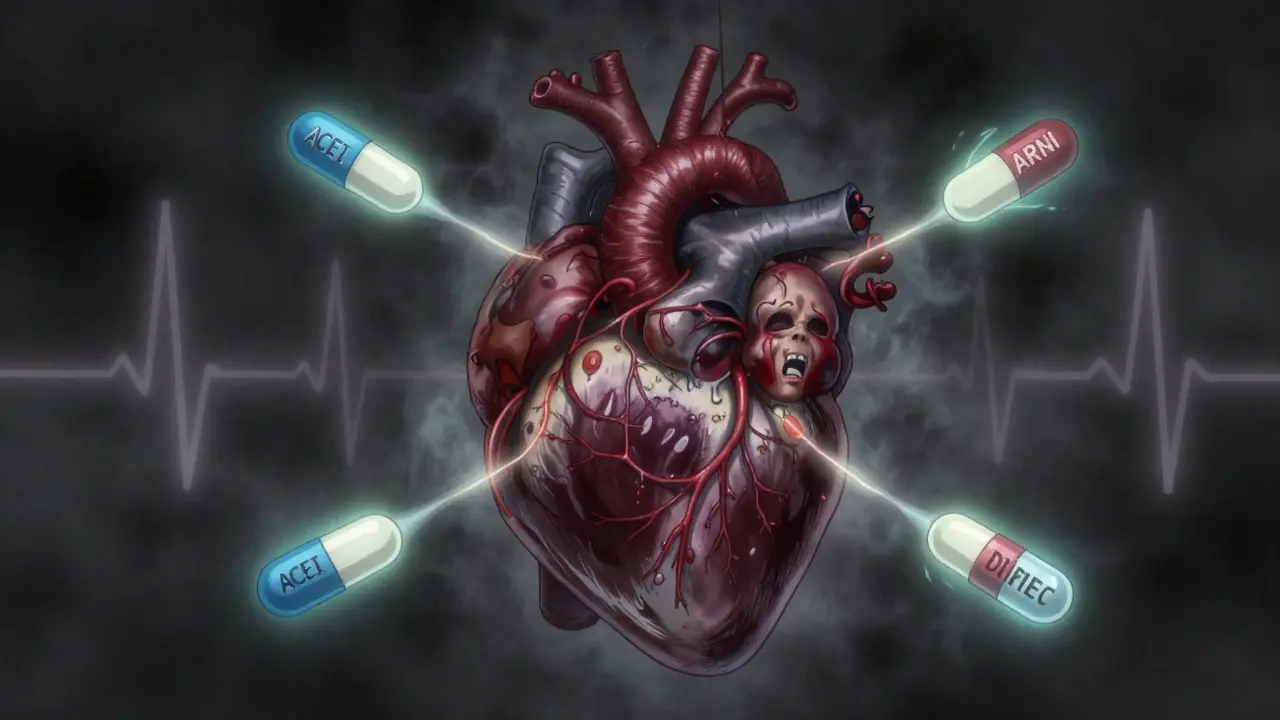
ACE inhibitors were the first heart failure meds proven to extend life. When enalapril showed a 27% drop in death risk in the 1987 CONSENSUS trial, it changed everything. These drugs block the enzyme that turns angiotensin I into angiotensin II, a hormone that tightens blood vessels and increases blood pressure. By stopping this, ACEIs reduce strain on the heart.
Common ones include lisinopril, enalapril, and ramipril. Doses start low-like 2.5 mg of lisinopril once a day-and slowly climb over weeks to target doses of 20-40 mg. The goal isn’t just to lower blood pressure; it’s to slow heart damage.
But they come with trade-offs. About 1 in 5 people get a dry, annoying cough. Some develop high potassium levels (hyperkalemia), which can be dangerous. A rare but serious side effect is angioedema-swelling of the face, lips, or throat. If that happens, you stop the drug immediately.
ARNI: The New Gold Standard
In 2015, everything shifted with the approval of sacubitril/valsartan (Entresto). This isn’t just another ACEI-it’s a hybrid. Sacubitril blocks neprilysin, an enzyme that breaks down helpful hormones like natriuretic peptides. These peptides help your body get rid of salt and water, relax blood vessels, and reduce heart stress. Valsartan blocks angiotensin receptors, just like an ARB.
The PARADIGM-HF trial, which followed nearly 8,400 people across 47 countries, showed ARNI reduced death and hospitalization by 20% compared to enalapril. That’s not a small win-it’s the biggest leap in heart failure treatment since beta blockers.
But you can’t just switch from an ACEI to ARNI. You must wait at least 36 hours after your last ACEI dose. Why? Because combining them too soon raises the risk of angioedema by half a percent. That’s rare, but serious enough to require caution.
Starting dose is 24/26 mg twice daily. Most people work up to 97/103 mg twice daily over 2-4 weeks. Blood pressure must stay above 100 mmHg systolic. If you’re dizzy or lightheaded, your doctor may slow the pace.
ARNI is now the first choice for most patients with reduced ejection fraction (HFrEF). The 2022 AHA/ACC/HFSA guidelines say it should replace ACEIs unless there’s a reason not to.
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards-how can slowing your heart help a failing heart? But in heart failure, a racing heart burns out the muscle faster. Beta blockers calm things down.
Three are proven: carvedilol, metoprolol succinate, and bisoprolol. These aren’t the same as beta blockers used for anxiety or high blood pressure. They’re specially formulated for heart failure and work slowly over months.
Start low-carvedilol at 3.125 mg twice daily, metoprolol at 12.5 mg once daily. Double the dose every 2-4 weeks only if your heart rate stays above 50 and you’re not getting worse. Many patients never reach the target dose because of fatigue or low blood pressure.
The benefits are real. The CIBIS-II trial showed bisoprolol cut death risk by 34%. The COPERNICUS trial found carvedilol cut death risk by 35% in severe cases. Long-term, some patients see their ejection fraction improve from 25% to 45%.
Side effects are common early on: tiredness, dizziness, low heart rate. Many patients quit because they feel worse before they feel better. But if you stick with it, most report better energy and less shortness of breath after 3-6 months.

Diuretics: Managing Fluid, Not Fixing the Heart
Diuretics don’t improve survival. They don’t fix the heart’s pumping power. But they make life bearable.
When the heart fails, fluid backs up into the lungs, legs, and belly. That’s what causes swelling, weight gain, and breathlessness. Diuretics flush that out.
Loop diuretics like furosemide, bumetanide, and torsemide are first-line. Furosemide starts at 20-80 mg daily. Torsemide might be more effective-studies show it reduces hospital readmissions by 18% compared to furosemide.
Thiazides like hydrochlorothiazide are used for mild cases or when loop diuretics aren’t enough. Spironolactone is special-it’s both a diuretic and a mineralocorticoid receptor antagonist (MRA). It reduces death by 30% in the RALES trial, but raises potassium risk.
People often complain about frequent urination. Some get leg cramps from low potassium or magnesium. Many patients on Reddit say they take potassium supplements or eat bananas and spinach to balance it out.
Key point: Diuretics are for symptom control. You take them when you feel puffy or short of breath. You don’t take them every day unless your doctor says so.
How These Drugs Work Together
Today’s standard is called quadruple therapy: ARNI (or ACEI/ARB), beta blocker, MRA (like spironolactone), and SGLT2 inhibitor (like dapagliflozin). Diuretics are added on top as needed.
Each drug tackles a different problem:
- ARNI/ACEI → reduces harmful hormones, lowers pressure
- Beta blocker → slows heart rate, prevents overwork
- MRA → blocks aldosterone, reduces scarring and fluid
- SGLT2 inhibitor → helps kidneys remove sugar and fluid, protects heart muscle
- Diuretic → removes excess water right now
Studies show this combo cuts death risk by 20% and hospital stays by 21%. But here’s the problem: only 35% of eligible patients get all four drugs within a year of diagnosis.
Real Patient Experiences
On PatientsLikeMe, 68% of users said they struggled to reach full beta blocker doses because of fatigue. 45% quit ACEIs because of the cough. But 82% of those who switched to ARNI kept taking it-because they could walk further and sleep better.
One Reddit user, u/HeartWarrior2020, said furosemide gave him terrible leg cramps until he started taking magnesium. Another, u/PumpFailure, switched from lisinopril to Entresto and noticed less shortness of breath in two weeks-but had to pee every hour.
Meanwhile, u/CHFSurvivor shared: “Carvedilol raised my ejection fraction from 25% to 45% over 18 months. It wasn’t easy, but it was worth it.”
Cost, Access, and Barriers
Generic lisinopril costs about $4 a month. Metoprolol is $6. ARNI? Around $550 without insurance. That’s why only 42% of community clinics use it, compared to 65% in big hospitals.
Medicare covers 85% of ARNI’s cost, but 78% of prescriptions need prior authorization. That means delays, paperwork, and sometimes patients never fill the prescription.
Renal problems, low blood pressure, and high potassium block many from reaching full doses. Doctors have to balance benefit and risk carefully.
What You Need to Monitor
If you’re on any of these drugs, your doctor should check:
- Potassium levels (target under 5.0 mmol/L)
- Creatinine (to watch kidney function)
- Blood pressure (must stay above 100 systolic for ARNI)
- Heart rate (shouldn’t drop below 50 bpm on beta blockers)
- Ejection fraction (repeat echo at 3-6 months)
Don’t skip these tests. High potassium can cause cardiac arrest. A 30% spike in creatinine means your kidneys are under stress.
What’s Next?
The FDA just approved ARNI for heart failure with mildly reduced ejection fraction (HFmrEF)-adding millions more patients who can benefit. SGLT2 inhibitors are now recommended for all types of heart failure, not just with diabetes.
Future drugs like vericiguat are being added to the mix. But the biggest challenge isn’t new science-it’s getting the right drugs to the right people. Too many still get outdated care.
Heart failure isn’t a death sentence anymore. With the right meds, taken correctly, people live longer, feel better, and stay out of the hospital. But only if they get the full treatment-and stick with it.


9 Comments
Akshaya Gandra _ Student - EastCaryMS
January 5, 2026 AT 07:17 AMi just read this and my brain is kinda blown… so ace inhibitors are like the OG heart failure drug? and now there’s this new combo thing called arni that’s better? and you have to wait 36 hours before switching? why not just make it one pill from the start?? also, why does everyone say ‘paradigm-hf trial’ like it’s a movie title??
Joseph Snow
January 6, 2026 AT 02:44 AMLet’s be honest-this whole ‘quadruple therapy’ is just pharmaceutical industry propaganda wrapped in clinical jargon. ACE inhibitors were fine for 30 years. Now suddenly we need ARNI, SGLT2 inhibitors, MRAs, and diuretics? Who’s paying for all this? Big Pharma. And don’t get me started on the ‘guidelines’-they change every five years like fashion trends. I’ve seen patients die from potassium spikes because doctors were too eager to push ‘evidence-based’ combos. This isn’t medicine-it’s a money pipeline.
Jacob Milano
January 6, 2026 AT 13:28 PMMy dad’s been on carvedilol and Entresto for two years now. He used to collapse after walking to the mailbox. Now he’s gardening, cooking, even teaching his grandkids how to fish. Yeah, he got dizzy at first. Yeah, he had to pee like a racehorse. But the difference? Night and day. I used to think heart failure meant slow death. Turns out, it just means slow *adaptation*. Don’t quit the meds because they feel weird at first. Stick with it. Your future self will high-five you.
Ashley Viñas
January 6, 2026 AT 14:23 PMOh wow. Another person who thinks ‘diuretics are just for symptoms’? Please. If you’re not monitoring potassium, magnesium, and renal function religiously, you’re not treating heart failure-you’re playing Russian roulette with a stethoscope. And if you’re taking furosemide without a banana in your pocket, you’re not a patient-you’re a walking electrolyte disaster. I’ve seen 72-year-olds in the ER with cardiac arrest because they ‘felt fine’ and skipped their labs. Don’t be that person.
en Max
January 7, 2026 AT 17:59 PMIt is, indeed, a remarkable evolution in the therapeutic paradigm of heart failure with reduced ejection fraction (HFrEF). The pharmacodynamic interplay between neprilysin inhibition and angiotensin receptor blockade-exemplified by sacubitril/valsartan-represents a paradigmatic shift from compensatory suppression to endogenous neurohormonal augmentation. Furthermore, the integration of SGLT2 inhibitors into the backbone regimen reflects a growing recognition of the renal-cardiac axis as a primary therapeutic target. However, the clinical implementation remains suboptimal, primarily due to socioeconomic and logistical barriers, including prior authorization delays and cost-related nonadherence, which disproportionately affect underserved populations. Systemic reform is required.
Allen Ye
January 9, 2026 AT 04:05 AMThink about it: we’re told to take five pills every day to keep a broken heart from giving out. But what is a heart, really? A pump? A muscle? Or is it the silent witness to decades of stress, grief, poor food, and sleepless nights? We treat the symptoms like they’re the problem-but the problem is a life lived in imbalance. These drugs don’t fix the heart. They buy time. Time to say sorry. Time to hold hands. Time to watch the sunset without gasping. Maybe the real cure isn’t in the pill bottle-it’s in the quiet moments between doses, when we remember why we’re still here.
Clint Moser
January 9, 2026 AT 16:19 PMyou know what they dont tell you? ARNI was tested on people who already had insurance and doctors who gave them 30-minute consults. what about the guy who works two jobs and can’t afford the $550? or the one who got the prescription but the pharmacy says ‘we need prior auth’ and waits 3 weeks? meanwhile his legs swell and he can’t breathe. and then they say ‘you didn’t follow the protocol’? lol. also… did you know the FDA approved ARNI for HFmrEF after a trial where 37% of patients dropped out because of dizziness? they just called it ‘adverse events’ and moved on. this isn’t science. it’s marketing with a lab coat.
Enrique González
January 11, 2026 AT 05:46 AMOne sentence: Keep taking the meds. Even when you feel worse. Your heart doesn’t quit. Neither should you.
Angie Rehe
January 11, 2026 AT 23:00 PMWow. So now we’re supposed to trust guidelines written by doctors who get paid by pharma? And you think people just ‘forget’ to take their potassium? No. They’re overwhelmed. They’re tired. They’re scared. And you’re out here lecturing them about bananas like it’s a parenting blog. I’ve seen patients cry because they can’t afford their ARNI. And now you’re telling them they’re irresponsible? Maybe the problem isn’t the patient. Maybe it’s a system that treats medicine like a luxury subscription. Wake up.