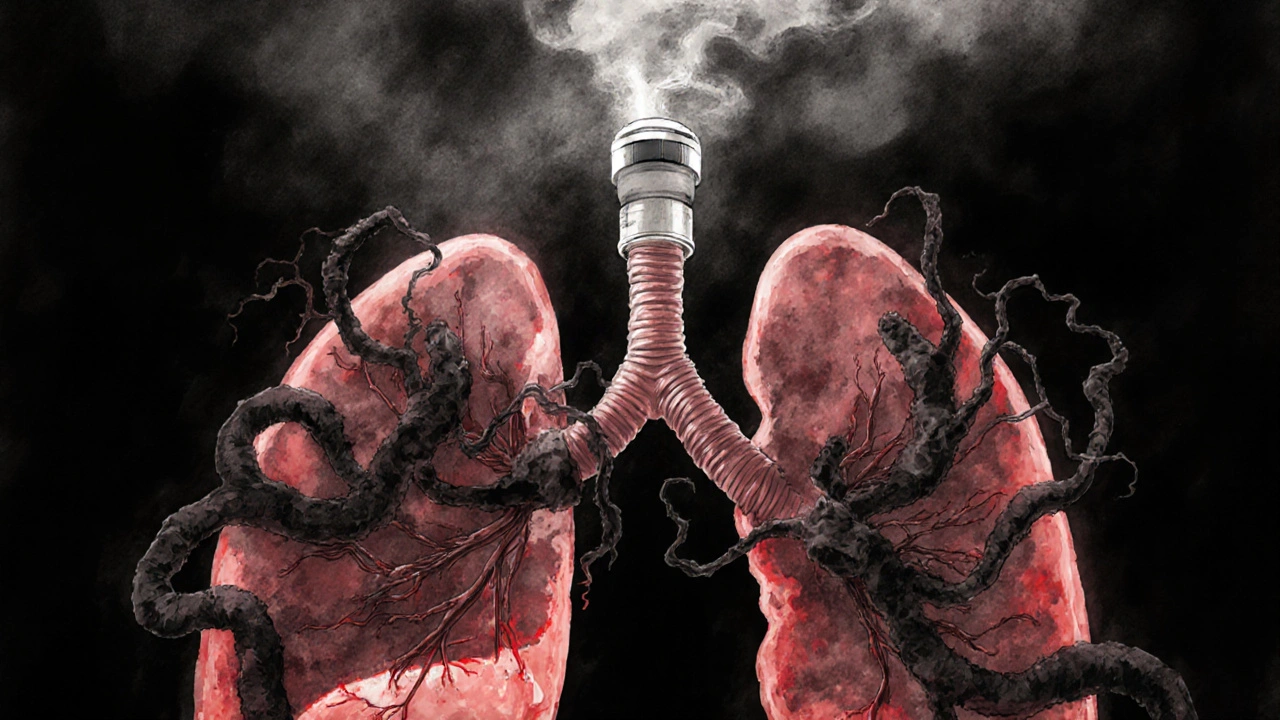
When bronchitis lingers - especially the chronic kind - your airways are swollen, sticky, and tight. You cough. You wheeze. You feel like you can’t catch your breath, even after weeks of rest. Over-the-counter remedies might ease the cough, but they don’t touch the inflammation underneath. That’s where beclomethasone comes in.
What beclomethasone actually does
Beclomethasone is an inhaled corticosteroid. It’s not a quick fix like a bronchodilator. You won’t feel better right after your first puff. But over days and weeks, it quietly reduces swelling in your bronchial tubes. Think of it like turning down the volume on your body’s inflammatory response. Instead of flooding your lungs with immune cells and mucus, it calms them down.
It’s the same class of drug used for asthma, and for good reason. Chronic bronchitis - often part of COPD - shares the same problem: inflamed, narrowed airways. Beclomethasone doesn’t cure it. But it makes breathing easier, reduces flare-ups, and lowers the chance you’ll end up in the hospital.
Why it’s used for bronchitis - and not always
Not every case of bronchitis needs beclomethasone. Acute bronchitis, usually from a virus, clears up on its own in a few weeks. Antibiotics don’t help much here, and neither do steroids. But if your bronchitis sticks around - three months or more, recurring for two years in a row - that’s chronic bronchitis. And if you also have wheezing, chest tightness, or a history of asthma, then inhaled steroids like beclomethasone are often recommended.
Guidelines from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) say inhaled corticosteroids should be considered for people with frequent exacerbations, especially if they’ve had two or more in the past year. Beclomethasone fits right into that category. It’s not for everyone with bronchitis, but for the right person, it’s one of the most effective tools they’ve got.
How it’s taken - and why technique matters
Beclomethasone comes in an inhaler. Not a pill. Not a syrup. You have to breathe it in, deep and slow. If you just spray it into your mouth and swallow, you’re wasting most of the dose. The drug needs to land on your airway lining, not your stomach.
Here’s how to use it right:
- Shake the inhaler well.
- Breathe out fully - away from the inhaler.
- Place the mouthpiece in your mouth and seal your lips.
- Press down on the canister as you start to breathe in slowly.
- Keep breathing in for 3-5 seconds, then hold your breath for 10 seconds.
- Wait 30 seconds before taking another puff, if prescribed.
Always rinse your mouth with water after each use. Leaving the steroid in your mouth increases your risk of thrush - a fungal infection that causes white patches and soreness. It’s simple to prevent, but many people forget.

What to expect - and what not to expect
Don’t expect instant relief. Beclomethasone works slowly. You might not notice a difference for 1-2 weeks. Some people take 4-6 weeks to feel the full benefit. That’s normal. It’s not a rescue inhaler. If you’re wheezing right now, you need a short-acting bronchodilator like salbutamol.
But over time, you’ll likely see fewer coughing fits, less mucus buildup, and fewer days where you feel too breathless to walk to the shop. Studies show people using inhaled corticosteroids like beclomethasone have up to 30% fewer flare-ups compared to those who don’t.
Side effects are usually mild. Hoarseness, throat irritation, and oral thrush are the most common. Serious side effects - like bone thinning or adrenal suppression - are rare at standard doses, especially since the drug is inhaled and doesn’t flood your whole body.
Who should avoid it
Beclomethasone isn’t for everyone. Avoid it if you have an active fungal, bacterial, or viral infection in your airways - like untreated tuberculosis or oral thrush - unless you’re also getting the right treatment for the infection. It suppresses local immune responses, so it can make infections worse.
If you’ve had an allergic reaction to beclomethasone or any other corticosteroid, don’t use it. Also, if you’re pregnant or breastfeeding, talk to your doctor. While inhaled steroids are generally considered safer than oral ones during pregnancy, you still need to weigh the risks.

Alternatives and combinations
Beclomethasone isn’t the only inhaled corticosteroid. Fluticasone, budesonide, and mometasone are others. They all work similarly, but some may be more affordable or come in different delivery systems.
Often, beclomethasone is combined with a long-acting bronchodilator like formoterol or salmeterol. These combinations - like Symbicort or Seretide - are common for people with more advanced COPD or asthma-like bronchitis. The steroid reduces swelling. The bronchodilator opens the airways. Together, they’re more effective than either alone.
For some, a short course of oral steroids might be used during a flare-up. But long-term oral steroids? That’s a last resort. They cause weight gain, high blood pressure, diabetes risk, and bone loss. Inhaled steroids like beclomethasone give you the benefit with far less risk.
Real-life impact
I’ve seen patients in Birmingham clinics who used to cancel plans because they couldn’t walk up the stairs without stopping. After starting beclomethasone, they’re back walking the dog, gardening, even taking short trips. It’s not magic. But it’s one of the few treatments that actually changes the course of chronic bronchitis - not just masking symptoms.
The key is consistency. Missing doses means inflammation creeps back. It’s not a drug you take when you feel bad. You take it every day, even when you feel fine. That’s how you keep your airways calm.
When to talk to your doctor
If you’ve been coughing for more than three weeks, or if you’re wheezing, feeling tight in the chest, or getting breathless with light activity - don’t wait. See your GP. They’ll check your lung function with a simple spirometry test. If they suspect chronic bronchitis or asthma overlap, they may prescribe beclomethasone.
Also, if you’re using your rescue inhaler more than twice a week, that’s a red flag. It means your inflammation isn’t under control. Beclomethasone might be the missing piece.
And if you’re using it and still struggling - or if you develop side effects like a persistent sore throat or vision changes - go back. Your dose might need adjusting. Or you might need a different combination.
Can beclomethasone cure bronchitis?
No, beclomethasone doesn’t cure bronchitis. It manages the inflammation that causes symptoms like wheezing, coughing, and shortness of breath. For chronic bronchitis - often linked to COPD - it helps reduce flare-ups and slow progression, but it doesn’t reverse lung damage. Stopping smoking and avoiding irritants are just as important.
How long does it take for beclomethasone to work for bronchitis?
It usually takes 1 to 2 weeks to start noticing a difference, and up to 6 weeks for the full effect. Unlike rescue inhalers, it doesn’t open airways immediately. It works by reducing long-term inflammation. Patience and consistent use are key.
Is beclomethasone the same as albuterol?
No. Beclomethasone is a corticosteroid that reduces swelling in the airways. Albuterol (salbutamol) is a bronchodilator that relaxes the muscles around the airways to open them up quickly. Beclomethasone is for daily control. Albuterol is for sudden symptoms. Many people use both.
Can you use beclomethasone for acute bronchitis?
Generally, no. Acute bronchitis is usually viral and lasts a few weeks. Steroids like beclomethasone aren’t recommended because they don’t speed up recovery and may increase the risk of side effects without benefit. They’re reserved for chronic cases with ongoing inflammation or asthma-like features.
What happens if I stop taking beclomethasone suddenly?
Stopping suddenly won’t cause withdrawal like some medications, but your inflammation will likely return. You may start coughing, wheezing, or having more flare-ups. Always talk to your doctor before stopping. They might suggest tapering slowly, especially if you’ve been on it for months or years.
If you’re managing chronic bronchitis, beclomethasone isn’t just another inhaler. It’s a tool that gives you back control - over your breathing, your routine, your life. But it only works if you use it right, consistently, and as part of a bigger plan. Quit smoking. Avoid pollution. Get your flu shot. And take your inhaler every day, even on the days you feel okay.


14 Comments
joe balak
November 2, 2025 AT 17:00 PMBeclomethasone works but it’s not magic. You still gotta quit smoking.
Neal Burton
November 2, 2025 AT 20:19 PMThe real issue isn’t the drug-it’s the medical-industrial complex pushing inhalers like they’re vitamins. No one talks about how pharma funds the GOLD guidelines. Beclomethasone isn’t a treatment-it’s a maintenance racket for people who won’t leave the city air.
I’ve seen patients on this for years, still coughing, still wheezing. The drug doesn’t fix the root cause. It just makes them feel like they’re doing something while their lungs slowly turn to ash.
And don’t get me started on the mouth rinse thing. That’s not hygiene-it’s damage control for a drug that shouldn’t be inhaled in the first place. Why not just give them oxygen tanks and call it a day?
The only reason this works at all is because people are desperate. Not because it’s effective. It’s palliative. Like putting a bandage on a severed artery.
And yet, doctors still prescribe it like it’s a cure. They’re not healers-they’re pharmacists with stethoscopes.
There’s a reason why traditional medicine in India and China uses herbal steam and breathing exercises. They don’t need synthetic steroids to calm inflammation. They just let the body breathe.
But no, we’d rather spend $200 a month on a canister that makes your throat raw and your teeth brittle.
It’s not medicine. It’s corporate appeasement.
Tamara Kayali Browne
November 4, 2025 AT 02:38 AMWhile the post presents a clinically accurate overview of beclomethasone’s role in chronic bronchitis management, it omits critical pharmacoeconomic data regarding cost-effectiveness compared to budesonide or fluticasone. Additionally, the omission of real-world adherence rates-particularly among elderly populations with comorbid cognitive decline-is a significant oversight. The recommended technique assumes dexterity and cognitive capacity that many patients lack. Without addressing these systemic barriers, the clinical utility of this intervention is overstated.
Nishigandha Kanurkar
November 4, 2025 AT 09:19 AMBECLoMETHASONE IS A GOVERNMENT-CONTROLLED TOXIN DESIGNED TO KEEP YOU DEPENDENT!!! THEY DON’T WANT YOU TO HEAL, THEY WANT YOU TO BUY INHALERS FOREVER!!! THE FDA IS IN BED WITH ASTRAZENECA!!! YOU THINK THEY’RE TEACHING YOU TO RINSE YOUR MOUTH TO PREVENT THRUSH?? NO!!! THEY’RE TRAINING YOU TO ACCEPT THE DRUG AS NORMAL!!! THEY’RE TURNING YOUR LUNGS INTO A SUBSCRIPTION SERVICE!!!
AND THE "GOLD GUIDELINES"?? THAT’S A CODE NAME FOR THE PHARMA CARTEL!!! THEY MADE UP COPD TO SELL DRUGS TO SMOKERS!!! YOUR CIGARETTES DIDN’T KILL YOU-THE INHALERS DID!!!
I USED TO HAVE CHRONIC BRONCHITIS-THEN I STOPPED THE INHALER AND ATE RAW GARLIC AND ATE A POUND OF GINGER DAILY-AND MY LUNGS CAME BACK!!! THEY DON’T WANT YOU TO KNOW THIS!!!
THEY’RE ALSO HIDING THAT BECLoMETHASONE CONTAINS NANO-PARTICLES THAT TRAVEL TO YOUR BRAIN AND MAKE YOU SLEEPY SO YOU DON’T ASK QUESTIONS!!!
Lori Johnson
November 5, 2025 AT 03:31 AMHey, I just started this last month and honestly? It’s been a game-changer. I used to cancel every weekend because I couldn’t walk to the mailbox without gasping. Now I’m walking the dog, even in winter. I know it doesn’t work fast, but I just kept at it.
And yes, I rinse my mouth like they said-no thrush, no hoarseness. It’s not glamorous, but it’s working.
My doc told me to think of it like brushing my teeth. You don’t stop because your mouth feels fine-you do it because you want to stay healthy.
I’m not a medical person, but this felt like the first thing that actually helped me breathe again. Not a cure, but a real tool.
Tatiana Mathis
November 6, 2025 AT 19:07 PMThis is one of the clearest, most balanced explanations of inhaled corticosteroid use in chronic bronchitis I’ve seen in a public forum. The distinction between acute and chronic is critical, and the emphasis on technique-especially the slow inhalation and breath hold-is often neglected in patient education. Many providers assume patients understand how inhalers work, but without proper demonstration and follow-up, efficacy plummets.
Additionally, the point about combination therapy is well-placed. For patients with frequent exacerbations, adding a LABA isn’t just additive-it’s synergistic. The data from the TORCH and POET trials support this approach.
It’s also worth noting that adherence is the single biggest predictor of outcomes, not the specific steroid chosen. Whether it’s beclomethasone, budesonide, or fluticasone, consistency matters more than brand.
And yes, the mouth rinse is non-negotiable. Thrush is preventable, not inevitable. Simple hygiene changes-like using a spacer if available and rinsing with water (not just swishing)-can eliminate 90% of local side effects.
Finally, the call to address smoking and pollution isn’t an afterthought-it’s the foundation. No inhaler can compensate for continued exposure to irritants. This post correctly frames beclomethasone as one component of a broader, patient-centered strategy.
Michelle Lyons
November 8, 2025 AT 00:27 AMThey say beclomethasone reduces inflammation… but what if inflammation is your body’s way of fighting something else? What if the real problem is the air you’re breathing? What if they’re hiding the truth about what’s in the inhaler? I read a blog once that said the propellant is laced with tracking microchips. They don’t want you to get better-they want you to be monitored. Every puff is a data point. That’s why they tell you to rinse. To hide the evidence.
And the "GOLD guidelines"? That’s not a medical group. That’s a front. I looked up the board members. Half of them work for drug companies. They wrote the guidelines to sell more inhalers. They don’t care about your lungs. They care about your monthly refill.
I stopped taking it. My cough got worse for a week… then it got better. Much better. I think my body was fighting the drug.
Cornelle Camberos
November 9, 2025 AT 00:52 AMWhile the post contains a superficially reasonable exposition of beclomethasone’s pharmacological profile, it fails to acknowledge the profound epistemological limitations inherent in contemporary pulmonology. The reliance on GOLD guidelines, which are themselves funded by pharmaceutical interests, constitutes a form of institutionalized pseudoscience. The notion that inflammation is the primary driver of chronic bronchitis is a reductive model that ignores the role of biofilm colonization, microbiome dysbiosis, and systemic oxidative stress. Furthermore, the assumption that inhalation delivers localized action is empirically dubious-systemic absorption is well-documented even at standard doses, particularly in elderly or obese patients. The omission of alternative modalities-such as high-dose vitamin D, N-acetylcysteine, and pulmonary rehabilitation-is not merely negligent; it is ideologically driven. This is not medicine. It is protocol.
Iván Maceda
November 9, 2025 AT 16:45 PM🇺🇸 This is why America’s healthcare is broken. We don’t fix causes-we sell pills. You’re telling me someone in Alabama with bronchitis from coal dust gets an inhaler instead of clean air laws? That’s not medicine. That’s capitalism with a stethoscope.
And yeah, I get it, the inhaler helps. But what about the people who can’t afford it? What about the ones without insurance? We turn a chronic condition into a profit loop. And we call it progress.
Real solution? Clean air. No coal plants. No factories spewing smoke near schools. But nah, that costs money. This? This costs $120 a month. And someone’s making bank.
Beclomethasone? Fine. But don’t act like it’s the answer. It’s a Band-Aid on a bullet wound.
John Rendek
November 10, 2025 AT 16:41 PMConsistency is everything. I was skeptical at first, but taking it every day-even when I felt fine-made all the difference. No magic, just discipline.
Sonia Festa
November 10, 2025 AT 17:32 PMBeclomethasone? More like be-clown-me-satone. I used it for a month and my throat felt like I’d swallowed a cactus. Rinsing? Yeah right, I just spit and hoped for the best. Still coughed like a chain-smoking raccoon. But hey, at least I looked like I was doing something. My grandma used turmeric and honey and lived to 92. Maybe we’re overcomplicating this.
Sara Allen
November 12, 2025 AT 00:55 AMi hate this thing so much. it makes my mouth all weird and i keep forgetting to rinse and then i get that white stuff and it hurts. why do i have to take it every day?? i feel fine most days. why can’t i just take it when i feel bad?? my doctor is so annoying about it. and now i have to buy a new inhaler every month and it costs a fortune. i just want to breathe without all this crap.
Vrinda Bali
November 13, 2025 AT 23:02 PMBeclomethasone is not a remedy-it is a surrender. In India, our ancestors used neem, tulsi, and steam with eucalyptus to clear the lungs. They did not rely on chemical chains manufactured in distant labs. The Western world has forgotten that the body can heal itself-if only we stop poisoning it with synthetic hormones disguised as medicine. The government, the doctors, the corporations-they all profit from your dependence. The truth? You were never meant to need this. You were meant to live in clean air. But the factories don’t care. And neither do they.
Cornelle Camberos
November 14, 2025 AT 02:46 AMIt is not surprising that the most effective interventions are those that are least profitable. The systemic failure to prioritize environmental regulation over pharmacological bandages reflects not a medical deficiency, but a moral one. The patient who requires beclomethasone is not merely ill-they are a casualty of policy failure. To prescribe this drug without simultaneously advocating for air quality reform is not clinical practice-it is complicity.