When you're breastfeeding and need to take a short-term medication-maybe antibiotics for an infection, painkillers after surgery, or even a short course of antidepressants-it’s natural to worry: Is my milk safe? Do I have to stop nursing? Should I throw away everything I’ve pumped? The short answer: Most of the time, you don’t need to stop. But you do need to store and label your milk correctly.
Why Labeling Matters More Than Ever
You’ve probably labeled your breast milk before: date, time, baby’s name. That’s the baseline. But when you’re on medication, that simple label isn’t enough. You’re not just tracking freshness-you’re tracking safety. Different medications enter your milk at different levels and times. Some peak within an hour. Others take 4-6 hours. If you mix milk pumped before, during, and after your dose, you risk giving your baby inconsistent doses of the drug.Here’s what you need to add to every container:
- The date and time you pumped
- Your baby’s name
- The name of the medication
- The dose you took (e.g., “500 mg amoxicillin”)
- The time you took the medication
Use waterproof labels and permanent ink. If you’re using storage bags, write directly on them with a marker designed for freezer use. If you’re using bottles, stick on a label and cover it with clear tape to prevent peeling. Don’t rely on memory-especially when you’re tired or dealing with a sick baby.
Storage Rules Don’t Change-But Your Batches Do
The standard storage guidelines still apply:- Room temperature (up to 77°F): 4 hours max
- Refrigerator (39°F): 4 days max
- Freezer (0°F): 6-12 months
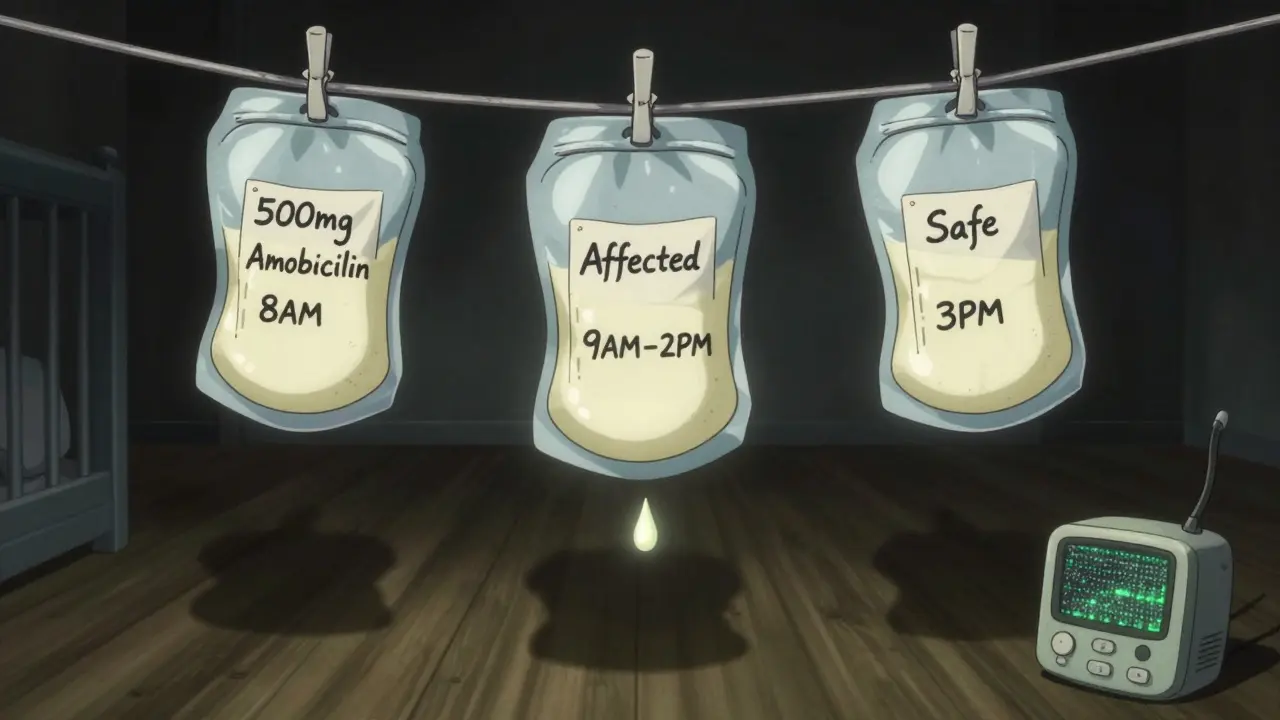
But here’s the catch: not all milk is the same. You need to separate your milk into batches based on when you pumped relative to your medication dose.
Let’s say you take a dose of ibuprofen at 8 a.m. The drug peaks in your milk around 1-2 hours later. So:
- Milk pumped before 8 a.m. = safe to use immediately (no medication)
- Milk pumped between 8 a.m. and 2 p.m. = medication-affected (store separately)
- Milk pumped after 2 p.m. = safe again (medication cleared)
That means you’ll have at least three separate batches. Label each clearly. Store them in different spots in your fridge or freezer. Don’t just toss them all together in one bag.
When Do You Actually Need to “Pump and Dump”?
Most moms think they need to dump milk every time they take a pill. That’s not true. In fact, fewer than 2% of medications require you to stop breastfeeding entirely.The American Academy of Pediatrics and the Academy of Breastfeeding Medicine agree: Most drugs transfer into milk in tiny, harmless amounts. Even strong medications like amoxicillin, acetaminophen, and sertraline are considered safe with no special precautions needed.
You only need to “pump and dump” if:
- Your doctor or pharmacist specifically says so (rare)
- You’re on a medication classified as L4 or L5 on the Hale scale (very high risk)
- You’re taking a drug not approved for breastfeeding, like certain chemotherapy agents or radioactive isotopes
For example, if you’re prescribed a short course of codeine, you might be told to avoid breastfeeding for 24-48 hours because it can convert to morphine in your body. In that case, you’d pump and dump for that window to maintain supply, then resume feeding with milk pumped after the window closes.
Don’t guess. Always check with your doctor or an IBCLC (International Board Certified Lactation Consultant). Use trusted resources like the Medications and Mothers’ Milk database or the MotherToBaby app (updated 2024) to verify safety.
How to Organize Your Milk Like a Pro
Managing multiple batches gets messy fast. Here’s how to keep it simple:- Use color-coded labels. Assign a color to each phase: green for “safe before meds,” yellow for “affected,” and blue for “safe after.”
- Use separate bins or containers. Keep your fridge or freezer organized: one section for pre-med milk, one for affected, one for post-med.
- Use small portions. Freeze milk in 2-4 ounce portions. That way, if you need to discard one batch, you’re not wasting a whole 8-ounce bag.
- Keep a log. Write down each dose time and the corresponding milk batches. A simple notebook or phone note works.
One mom on Reddit shared her system: she used sticky notes with the medication name and time on the front of each bag, and a small dry-erase board on her fridge showing the medication schedule. She said it cut her stress in half.

What to Do When You’re Away From Home
Traveling? Working? Going to the doctor? You still need to manage your milk.Use an insulated cooler with frozen ice packs. The CDC says it’s safe for up to 24 hours. But here’s the trick:
- Keep your pre-med milk in one insulated bag.
- Keep your affected milk in another.
- Label each bag with the same details: medication, time, date.
Don’t let your cooler sit in a hot car. If you’re at work, ask your HR department if you can use the fridge in the break room. Most employers are legally required to provide a clean, private space to pump-but they’re not always aware they need to provide storage space too. Ask.
Common Mistakes (And How to Avoid Them)
Based on surveys of over 500 breastfeeding mothers taking temporary medications, these are the top errors:- Mixing batches. 52% of moms accidentally combined affected and clean milk. Result? Confusion, wasted milk, or worse-baby gets unintended medication.
- Throwing away too much. 41% dumped milk unnecessarily because they didn’t know the medication was safe. You don’t need to dump unless told to.
- Not labeling the medication. 68% forgot to write down the drug name or dose. That’s a recipe for disaster if you’re not the one feeding the baby.
- Waiting too long to pump. If you’re told to pump and dump, wait 1-2 hours after your dose to start. Pumping too soon means you’re just recycling the drug.
Pro tip: If you’re unsure, err on the side of caution-but don’t panic. Call your lactation consultant. Most hospitals have them on call 24/7.
What Happens to the Milk You Discard?
If you do need to pump and dump, don’t feel guilty. It’s not wasted. You’re protecting your supply so you can keep feeding later. The milk you discard doesn’t harm your body-it just doesn’t go to your baby. Your body will keep producing based on demand.Some moms donate discarded milk to milk banks-but only if it’s collected under sterile conditions and you’re not on medication. If you’re on meds, even safe ones, milk banks won’t accept it. That’s why labeling matters: if you accidentally donate affected milk, it could harm another baby.

When to Call Your Doctor
You don’t need to call for every pill. But reach out if:- You’re prescribed something new and the label doesn’t mention breastfeeding
- You feel your baby is acting differently-sleepier, fussier, less interested in feeding
- You’re unsure how long to wait after a dose
- You’re taking multiple medications at once
Don’t rely on Google. Use the Medications and Mothers’ Milk app or call MotherToBaby at 1-866-626-6847. They’re free, confidential, and staffed by pharmacists and lactation experts.
Future Changes Are Coming
The FDA is planning to require medication labels to include breastfeeding storage instructions by 2025. That’s a big step. Right now, only 37% of prescriptions include any guidance at all. But until then, you’re the expert on your body and your baby. Learn the rules, label everything, and trust your instincts.Do I have to throw away all my milk when I take medicine?
No, not unless your doctor specifically says so. Most medications, including common ones like ibuprofen, amoxicillin, and acetaminophen, are safe to take while breastfeeding. You only need to discard milk if you’re on a rare high-risk drug or if your provider advises it. The key is to label your milk correctly and store affected batches separately.
How long should I wait after taking medicine before breastfeeding?
It depends on the medication. For most drugs, the peak level in breast milk happens 1-3 hours after taking it. Waiting 2-4 hours after your dose gives your body time to clear most of the drug from your milk. If you’re unsure, check a trusted source like MotherToBaby or ask your pharmacist. Never guess-especially with painkillers or antibiotics.
Can I freeze milk that was pumped while on medication?
Yes, you can freeze milk pumped during medication use-as long as the medication is safe for breastfeeding. If the drug is approved for nursing, freezing it is perfectly fine. Just make sure it’s labeled with the medication name, dose, and time. If the drug requires you to pump and dump, don’t freeze it. Always confirm safety before storing.
What if I forget to label my milk?
If you’re unsure when the milk was pumped or whether you were on medication, it’s safest to discard it. But don’t panic-this happens to everyone. Use it as a reminder to set a phone alert next time you take a pill. Consider using color-coded labels or a milk-tracking app to prevent future mix-ups. Your baby’s safety is worth the extra minute.
Is it safe to give my baby milk from a different day if I’m on meds?
Yes, as long as it was pumped before you started the medication or after the drug has cleared from your system. Always check your labels. Milk from before your first dose is safe. Milk from after the last dose, once the medication has cleared (usually 1-5 half-lives), is also safe. Never mix milk from different phases unless you’re certain they’re both clean.




10 Comments
Ted Conerly
January 10, 2026 AT 15:45 PMLabeling your milk with the med name and time is non-negotiable. I saw a mom mix batches once and her baby got a weird reaction-turned out it was the antibiotic she didn’t label. Don’t be that person. Write it down. Every time. No excuses.
Ashlee Montgomery
January 10, 2026 AT 19:16 PMI used to think pumping and dumping was the default. Then I learned that 98% of meds are fine. The real enemy isn’t the medication-it’s the fear that gets passed around like gossip. Do your research. Talk to an IBCLC. Your baby doesn’t need perfect milk-they need you sane and fed.
Ian Cheung
January 12, 2026 AT 18:09 PMColor coding changed my life green for safe before yellow for the window blue for safe after. I even made a little chart for my partner so he didn’t have to guess. Took five minutes to set up. Saved me from a million panic moments.
Lisa Cozad
January 14, 2026 AT 07:24 AMMy hospital didn’t even tell me about MotherToBaby until I asked. They handed me a pamphlet with outdated info. Don’t rely on the system. Bookmark the app. Save the number. You’re your baby’s best advocate.
Jay Amparo
January 16, 2026 AT 06:47 AMIn my village in Kerala we never labeled milk. We just knew-by smell, by time, by instinct. But here, in this world of spreadsheets and QR codes, I get it. It’s not about distrust-it’s about shared responsibility. If someone else feeds your baby, they deserve to know what they’re giving.
Saumya Roy Chaudhuri
January 18, 2026 AT 03:13 AMAnyone who doesn’t use waterproof labels is just asking for disaster. I once saw someone use a regular Sharpie on a bag-it smudged in the freezer. The baby got a 12-hour dose of amoxicillin because the label vanished. Don’t be that person. Use freezer-grade markers. It’s not hard.
Jake Nunez
January 20, 2026 AT 02:26 AMMy wife took Zoloft for three weeks after our daughter was born. We labeled every bag. We froze them separately. We used a notebook. And guess what? Our baby never missed a beat. The system works. You don’t need to be perfect-just consistent.
Mario Bros
January 21, 2026 AT 19:19 PMJust threw out 4 oz of milk because I forgot to label it. Felt awful. Now I have a sticky note on my pump: ‘Write it before you store it.’ Worth the extra 10 seconds. No regrets.
Faith Edwards
January 21, 2026 AT 20:02 PMIt is profoundly disheartening to witness the casual disregard for empirical safety protocols in the contemporary lactation landscape. One cannot, in good conscience, permit the conflation of anecdotal experience with pharmacological exigency. The integrity of infant nutrition is not a matter of convenience-it is a bioethical imperative. One must, therefore, adhere to the strictest nomenclatural and temporal delineations, lest one become complicit in the erosion of neonatal pharmacovigilance.
Christine Milne
January 21, 2026 AT 20:32 PMWhy are we even talking about this? In America, we’ve turned breastfeeding into a high-stakes science experiment. Back in my day, moms just fed their babies and didn’t worry about every pill. Now we’re labeling milk like it’s a chemical compound. It’s overkill. If your kid gets a little ibuprofen in their milk, they’ll be fine. Stop being so anxious.