Diagnosis: Understanding How Medications and Conditions Are Identified
When you hear the word diagnosis, the process of identifying a disease or condition based on symptoms, tests, and medical history. Also known as medical identification, it's not just about naming what’s wrong—it’s about figuring out what will fix it without making something else worse. A wrong diagnosis can turn a helpful drug into a dangerous one. Take bipolar depression—it looks like regular depression, but giving someone with bipolar disorder a standard antidepressant can trigger mania or seizures. That’s why diagnosis isn’t a one-time event. It’s a chain: symptoms lead to tests, tests lead to drug choices, and drug choices lead to side effects that change how you respond.
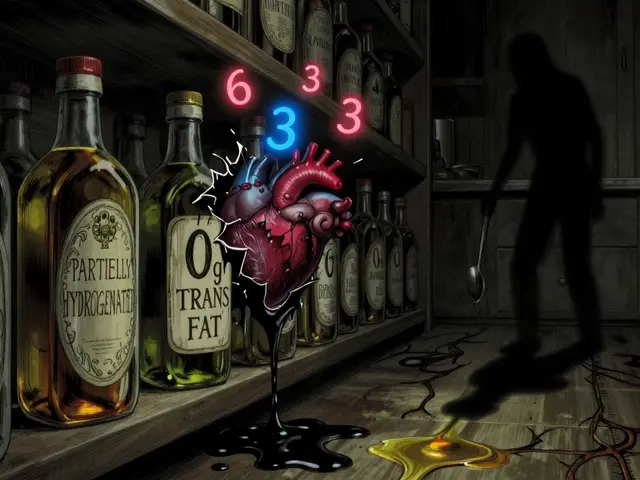
That’s where medication side effects, unintended reactions to drugs that can mimic or mask other conditions come in. Bupropion might help with depression, but if it causes insomnia or anxiety, your doctor might think you’re dealing with an anxiety disorder instead. Tricyclic antidepressants can fog your thinking, making it look like early dementia. Even something as simple as acid-reducing pills can hide the real problem—like poor absorption of HIV meds—because they change how your body handles other drugs. And then there’s drug interactions, when one medication changes how another works in your body. Grapefruit juice with heart meds. Goldenseal with liver enzymes. Alcohol with diabetes pills. These aren’t edge cases. They’re common traps that mess up diagnosis because the symptoms look like new diseases, not side effects.
Then there’s patient adherence, how consistently someone takes their meds as prescribed. If you stop taking statins because you heard they cause ALS (they don’t), your doctor might think your cholesterol is out of control for a different reason. If you skip your seizure meds during pregnancy because you’re scared of birth defects (and don’t tell your doctor), they might misread your seizures as something else entirely. Even switching from brand to generic can lower adherence—not because generics don’t work, but because the pill looks different, and you think it’s not the same. That’s not just a compliance issue. It’s a diagnostic blind spot.
And behind all of this is pharmacokinetics, how your body absorbs, moves, and breaks down drugs. Two drugs might have the same active ingredient, but if one hits your bloodstream faster (Cmax) or stays longer (AUC), your body reacts differently. That’s why generic approval isn’t just about price—it’s about matching the exact way the original drug behaves. If the numbers don’t fall between 80% and 125%, it’s not equivalent. And if your body doesn’t get the same exposure, your diagnosis could be off.
Diagnosis isn’t a checklist. It’s a conversation between your symptoms, your meds, your habits, and your body’s response. The posts below don’t just list conditions or drugs—they show how these pieces connect. You’ll find real stories about misdiagnoses, hidden interactions, adherence traps, and how small changes in how a drug works can change everything. Whether you’re a patient trying to understand why your treatment isn’t working, or just someone who wants to know how medicine really works, this is where the pieces come together.

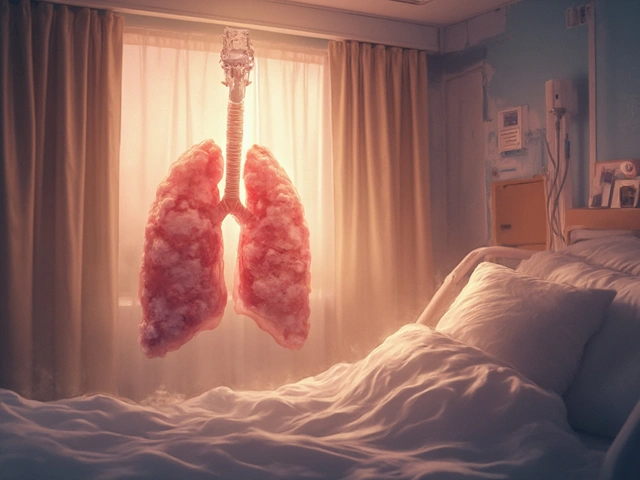
Lactose Intolerance: How to Get Diagnosed and Eat Without Pain
Learn how lactose intolerance is diagnosed with breath tests or elimination diets, and discover practical ways to manage symptoms without cutting out all dairy. Get real tips on what to eat, hidden lactose sources, and when to see a doctor.