Offending Medication – Risks, Side Effects, and Management
When talking about offending medication, a drug that causes unexpected harm or outweighs its benefits for a patient. Also known as problematic drug, it often shows up in adverse drug reaction, an unwanted, harmful response that occurs at normal doses, drug side effects, the predictable unwanted outcomes that may vary in severity, and can lead to medication intolerance, a situation where a patient cannot tolerate the drug without significant discomfort. Understanding these pieces helps you spot the culprits before they cause bigger problems.
Why Knowing Offending Medications Matters
Every day clinicians face drug interactions, situations where two or more substances affect each other's action. A harmless pill can become an offending medication the moment it meets another drug, a food, or a health condition. For instance, statins taken daily may turn into a muscle‑pain trigger when combined with certain antibiotics. Recognizing that interaction early cuts down on hospital visits and lets doctors adjust dosing before the harm spreads.
Adverse drug reactions are not just a statistic; they’re a real‑world pain point. Studies from major hospitals show that up to 15 % of emergency admissions involve an ADR linked to an offending medication. These reactions often share common attributes: sudden onset, reproducibility after re‑exposure, and a clear temporal link to the drug start. By cataloguing which drugs most frequently cause ADRs, you can prioritize monitoring those high‑risk agents.
Side effects can range from mild nausea to life‑threatening bleeding. The difference between a tolerable side effect and a red‑flag offending medication usually hinges on severity and persistence. Take local anesthetics in cosmetic dentistry: while lidocaine usually numbs without issue, a rare allergy can turn a routine procedure into a severe systemic reaction. Knowing the side‑effect profile lets you weigh the benefits against the risk for each patient.
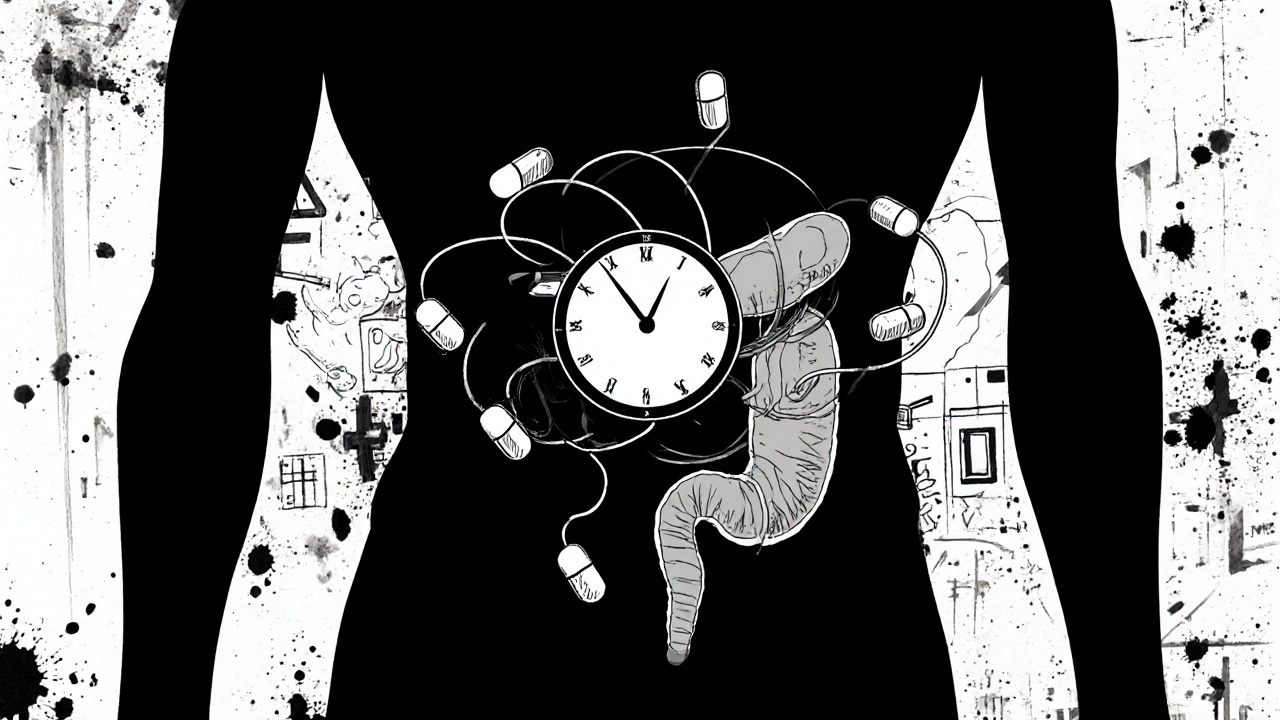
Medication intolerance often shows up as chronic discomfort—think persistent headaches after starting a new migraine pill or gastrointestinal upset with a common antibiotic. Unlike a clear‑cut allergy, intolerance can be subtle, making the offending medication harder to spot. Tracking patient reports and adjusting the regimen early can prevent escalation into full‑blown adverse events.
Drug interactions act as the hidden engine behind many offending medication cases. A common example is the interaction between certain blood thinners and over‑the‑counter NSAIDs, which can amplify bleeding risk dramatically. By mapping out known interaction pathways, clinicians can flag potential offending scenarios before prescribing, saving time and avoiding unnecessary lab work.
Patients with multiple health conditions—such as diabetes, hypertension, or autoimmune disorders—are especially vulnerable. Polypharmacy raises the odds that one drug will become an offending medication. Regular medication reviews, using tools like interaction checkers, empower both doctors and patients to prune risky drugs and replace them with safer alternatives.
Finally, proactive strategies—dose adjustments, switching to a different drug class, or employing non‑pharmacologic therapies—can neutralize the threat of offending medications. The articles below dive into real‑world cases, from alternate‑day statin dosing to safer local anesthetic choices, giving you actionable insights to keep your prescribing sharp and patient‑focused. Explore the collection to see how you can spot, manage, and replace offending medications before they cause trouble.
Medication‑Induced Severe Pancreatitis: Warning Signs and Treatment
Learn how to spot medication‑induced severe pancreatitis, identify high‑risk drugs, and follow a step‑by‑step treatment plan that can save lives.