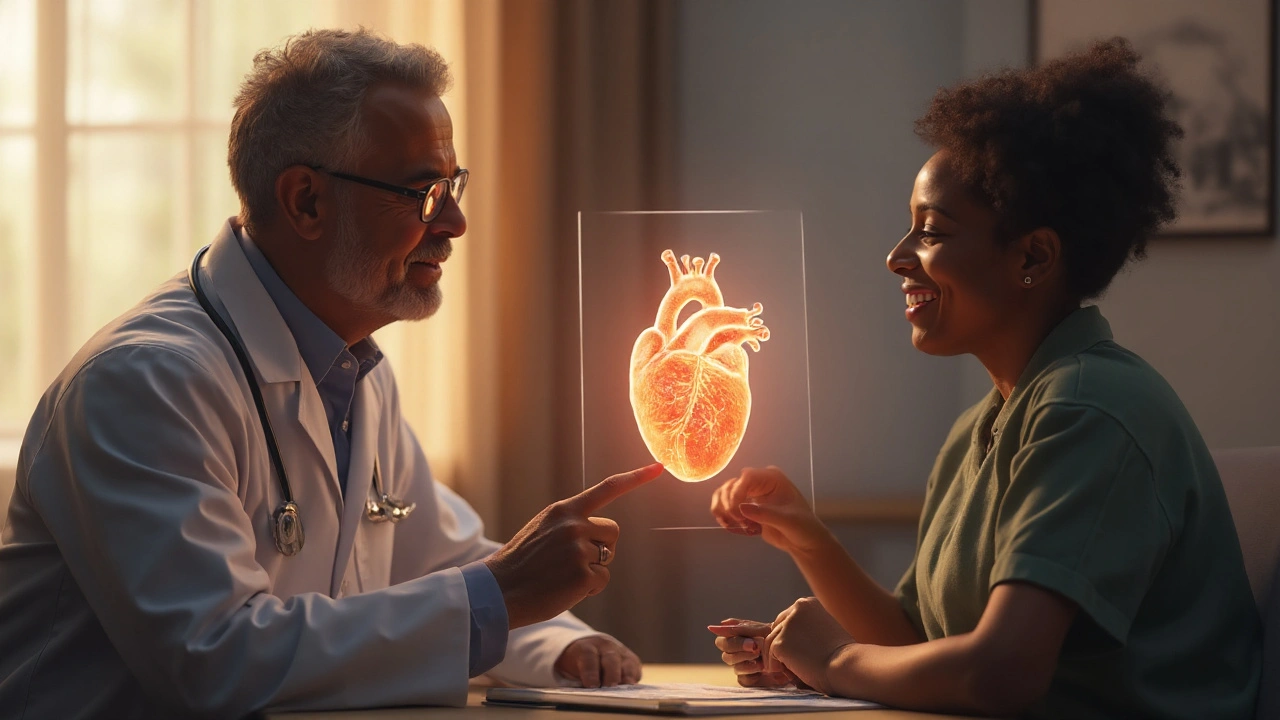
Treatment for Left Ventricular Failure: What Works and How to Start
If your doctor told you you have left ventricular failure (LVF), you might feel overwhelmed. The good news is that most people can slow the disease, feel better, and live longer with the right mix of medicines, lifestyle tweaks, and, when needed, devices. Below is a plain‑language guide that walks you through the most common treatment steps.
Medications commonly used
The backbone of LVF care is a set of drugs that lower the heart’s workload and improve its pumping ability. Here’s what you’ll likely hear about:
- ACE inhibitors or ARBs – These relax blood vessels, making it easier for blood to flow. Most patients start on an ACE inhibitor (like lisinopril) and switch to an ARB (like losartan) if they can’t tolerate it.
- Beta‑blockers – Drugs such as metoprolol or carvedilol slow the heart rate and reduce harmful stress hormones. They take a few weeks to show benefit, so patience matters.
- Diuretics – Loop diuretics like furosemide help get rid of excess fluid that builds up in the lungs and legs. You’ll notice less swelling and easier breathing.
- Mineralocorticoid receptor antagonists – Spironolactone or eplerenone block a hormone that makes the heart stiff. They are added when the disease progresses.
- ARNI (angiotensin receptor‑neprilysin inhibitor) – Sacubitril/valsartan combines two actions and has become a go‑to for many LVF patients.
Doctors may also prescribe digoxin for rhythm control or hydralazine–nitrate combo for certain groups, especially African‑American patients. Always discuss side effects and how to take each pill correctly.
Lifestyle steps that help
Medicine works best when you back it up with daily habits that ease the heart’s job.
Watch your sodium – Aim for less than 2,000 mg a day. Read food labels, skip table salt, and choose fresh over processed foods.
Control fluid intake – Your doctor might set a limit (often 1.5–2 L per day) to prevent overload.
Stay active – Light aerobic exercise, like walking 20‑30 minutes most days, improves circulation and heart strength. Start slow and let your cardiologist clear you before any new routine.
Weight management – Even a small loss (5‑10 % of body weight) can lower heart strain. Focus on balanced meals with lean protein, whole grains, and lots of veggies.
Quit smoking & limit alcohol – Both hurt the heart. Resources such as quit‑lines or support groups can boost success.
Regular check‑ups are key. Your doctor will monitor blood pressure, kidney function, and electrolytes to fine‑tune doses. If symptoms worsen (more shortness of breath, swelling, or fatigue), call your provider right away.
In advanced cases, device therapy may be recommended. Cardiac resynchronization therapy (CRT) can coordinate heart beats, while a left ventricular assist device (LVAD) takes over part of the pumping work. These options are discussed when medication and lifestyle changes aren’t enough.
Bottom line: Treating left ventricular failure is a team effort between you, your doctor, and the medicines you take. Stick to the prescribed regimen, adopt the simple lifestyle habits above, and keep an eye on any changes. With consistent care, many people see a real boost in energy and daily function.
Left Ventricular Failure: Causes, Symptoms & Treatment Guide
Learn what left ventricular failure is, why it happens, common warning signs, and how doctors treat it with medication, devices, and lifestyle changes.