Many people believe they’re allergic to penicillin or other medications because they had a rash or stomach upset years ago. But here’s the truth: 9 out of 10 people who think they have a drug allergy don’t actually have one. Skin testing can prove it - and it could change how you’re treated the next time you need antibiotics.
What Is Drug Allergy Skin Testing?
Drug allergy skin testing is a safe, quick way to find out if your body reacts to a specific medication. It doesn’t test for all drugs - only the ones you’ve been told you’re allergic to, like penicillin, cephalosporins, or certain painkillers. The test looks for immediate allergic reactions, which happen within minutes to an hour after exposure. These include hives, swelling, trouble breathing, or anaphylaxis.
There are three main types of skin tests used for drugs:
- Skin prick test (SPT): A tiny drop of the drug solution is placed on your skin, then the surface is gently pricked with a small needle. It feels like a light mosquito bite.
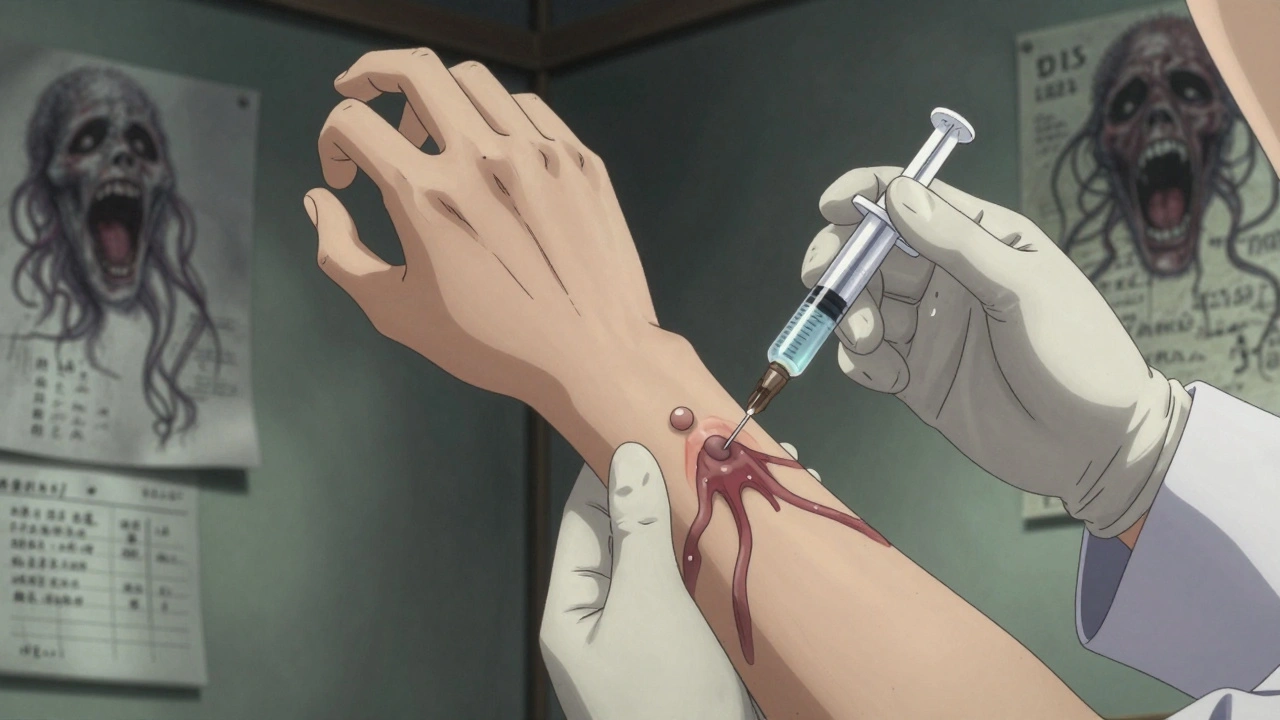
- Intradermal test (IDT): A small amount of the drug is injected just under the skin, creating a tiny bubble. This is more sensitive than the prick test.
- Patch test: A patch with the drug is taped to your back for 48 hours. This checks for delayed reactions, like rashes that appear days later.
Most drug allergy testing uses the first two - SPT and IDT - because they’re best at catching immediate reactions. Patch tests are used only if your reaction happened more than a few hours after taking the drug.
How Accurate Is It?
For penicillin and related antibiotics, skin testing is highly accurate. If both the skin prick and intradermal tests are negative, there’s a 95% to 98% chance you’re not truly allergic. That means you can safely take penicillin or amoxicillin in the future without fear.
But accuracy drops for other drugs. For cephalosporins, sulfa drugs, or NSAIDs like ibuprofen, skin tests are less reliable - sometimes only 30% to 50% accurate. That’s why doctors sometimes follow up with a drug challenge: giving you a small, controlled dose under supervision to see if you react.
One big reason skin testing isn’t used more? Many doctors don’t do it. In the U.S., only 30% to 40% of people with suspected penicillin allergies get tested. In countries like France and Germany, that number is over 65%. The good news? Hospitals that started routine testing saw a 30% drop in broad-spectrum antibiotics - meaning fewer side effects, lower costs, and less risk of dangerous infections like C. diff.
What Happens During the Test?
You’ll sit in a clinic or hospital allergy unit. The area on your arm or back will be cleaned. A nurse or allergist will mark spots with a permanent marker - each one for a different substance.
They’ll test three things:
- Positive control: Histamine. This should make your skin red and itchy - if it doesn’t, the test might not work.
- Negative control: Saline (salt water). Your skin shouldn’t react at all.
- Drug solution: The medicine you’re being tested for, diluted in saline.
For the skin prick test, the allergist lightly taps the skin with a needle. No blood. No deep poke. Just enough to let the solution get into the top layer. You’ll wait 15 to 20 minutes. If there’s a reaction, you’ll see a red, raised bump - like a mosquito bite - at that spot.
If the prick test is negative, they’ll move to the intradermal test. A tiny needle injects 0.02 to 0.05 milliliters of the drug just under the skin. Again, you wait 15 to 20 minutes. A positive result means the bump grew by 3 millimeters or more.
Some people feel a slight sting during the intradermal test - like a quick pinch. Others say it’s just uncomfortable. One patient on Reddit described it as “a stinging sensation that lasted 2 to 3 minutes per site.” But no one gets sick from the test. The amount of drug used is microscopic - not enough to enter your bloodstream in a harmful way.
What Should You Do Before the Test?
This is critical: Stop all antihistamines 5 to 7 days before testing. That includes:
- Over-the-counter pills like Zyrtec, Claritin, Allegra, Benadryl
- Nasal sprays like Flonase or Nasacort
- Eye drops for allergies
If you’re taking these for eczema, hives, or hay fever, talk to your doctor. They might switch you to something that doesn’t interfere, like a steroid cream. Skipping this step can give you a false negative - meaning the test says you’re not allergic when you actually are.
Also, avoid caffeine, alcohol, and heavy exercise the day before. These can make your skin more reactive and mess with the results.
What If the Test Is Positive?
If your skin reacts, it means your immune system recognizes the drug as a threat. You’ll be told to avoid that medication in the future. Your doctor will give you a medical alert bracelet or note in your chart.
But here’s the twist: A positive test doesn’t always mean you’ll have a bad reaction again. Some people had a rash years ago that wasn’t even an allergy - maybe it was a virus or side effect. The skin test confirms if your body truly treats the drug like an invader.
If you’re allergic to penicillin, you might still be able to take other antibiotics safely. For example, if you’re allergic to amoxicillin, you might tolerate cefdinir or azithromycin just fine. Your doctor will help you pick alternatives.
What If the Test Is Negative?
A negative result is powerful. It means you’re likely not allergic. Many patients are shocked when they hear this - they’ve avoided penicillin for 20 years, only to find out they could have taken it safely.
After a negative test, your doctor may recommend a drug challenge: giving you a full dose of the antibiotic in the clinic while watching you closely. If you don’t react, you’re officially “delabeled.” That means your medical records get updated, and you’re no longer flagged as allergic.
One case from the Cleveland Clinic involved a 45-year-old woman who’d avoided all penicillin-based drugs since childhood. After negative skin tests and a successful amoxicillin challenge, she was able to take the antibiotic for a tooth infection - avoiding expensive, stronger drugs she didn’t need.
Who Should Get Tested?
You should consider skin testing if:
- You were told you’re allergic to penicillin or another antibiotic
- You had a reaction years ago and aren’t sure what caused it
- You’ve avoided certain drugs and now need them for an infection
- You’re scheduled for surgery and need antibiotics
- You’re pregnant and need safe antibiotics
It’s especially important if you’ve been labeled allergic but never had a serious reaction like swelling, trouble breathing, or anaphylaxis. Rashes alone - especially if they came days after taking the drug - are often not true allergies.
What Are the Risks?
Skin testing is very safe when done by trained professionals. The biggest risk is a local reaction - itching, redness, swelling at the test site. That’s normal if it’s positive.
Very rarely, someone might have a more serious reaction. That’s why testing is always done in a clinic with emergency equipment on hand. Staff are trained to treat anaphylaxis with epinephrine, oxygen, and IV fluids.
You should never get tested if:
- You’re having an active allergic reaction
- You have uncontrolled asthma
- You’re on beta-blockers (these can interfere with emergency treatment)
And no, you can’t do this at home. There are no FDA-approved home kits. Only licensed allergy specialists should perform these tests.
What’s New in Drug Allergy Testing?
In 2022, the European Medicines Agency approved standardized penicillin test kits - a big deal. Before, labs made their own solutions, and results varied. Now, every clinic uses the same reliable mix.
Researchers are also working on test solutions for other drugs like ciprofloxacin and vancomycin. Early trials show promise. In January 2023, the National Institute of Allergy and Infectious Diseases updated guidelines to include opioid allergy testing - something once thought too risky.
And hospitals are catching on. A 2023 study in JAMA Internal Medicine found that hospitals with formal allergy testing programs had 22% fewer cases of C. diff infection. Why? Because they stopped overusing broad-spectrum antibiotics.
Why This Matters for You
If you’ve been told you’re allergic to a common drug, you’re probably not alone. But you might be mislabeled. That means you’re getting less effective, more expensive, or riskier medications than you need.
Drug allergy skin testing isn’t just about avoiding rashes. It’s about getting the right treatment, avoiding hospital stays, and reducing antibiotic resistance. It’s simple, safe, and fast - and it could change your health for the rest of your life.
Ask your doctor: “Could I be tested to confirm if I’m really allergic?” If they say no, ask for a referral to an allergist. You’ve got nothing to lose - and a lot to gain.





13 Comments
Girish Padia
December 2, 2025 AT 13:51 PMI've seen too many people get labeled allergic just because they got a rash after taking antibiotics as a kid. Most of the time it wasn't even the drug-it was a virus they had at the same time. Skin testing should be standard, not optional.
Saket Modi
December 3, 2025 AT 16:10 PMUgh, another ‘just get tested’ post. 😴 I’ve been told I’m allergic to penicillin since I was 12. Why should I trust some doctor with a needle when I’ve been fine avoiding it for 30 years?
Chris Wallace
December 3, 2025 AT 16:46 PMIt’s wild how many people carry around medical labels from childhood that just don’t hold up. I had a cousin who avoided all penicillin-based meds for decades until she got tested-turns out she was never allergic. She got her first amoxicillin prescription at 48 for a sinus infection and didn’t even flinch. It’s not just about avoiding rashes-it’s about not getting stuck with last-resort antibiotics that wreck your gut. And honestly, that’s a huge deal if you’ve ever had C. diff.
John Webber
December 3, 2025 AT 21:31 PMwhy do docs even bother with this? its just a waste of time. i dont trust no skin test. what if they mess up? then i die. i just dont take the meds. simple.
Kristen Yates
December 5, 2025 AT 04:34 AMI’m 52 and was told I’m allergic to penicillin after a mild rash at age 8. I’ve avoided it ever since. I never thought to question it until my doctor mentioned skin testing last year. I got tested-negative. I took amoxicillin for a UTI last month. No reaction. I feel like I’ve been living with a phantom label for 44 years.
Michael Campbell
December 5, 2025 AT 15:02 PMBig Pharma pushed this to sell more expensive antibiotics. Skin tests? Too cheap. They want you on the $500-a-pill stuff. Watch the data-they’ll disappear if testing becomes common.
alaa ismail
December 6, 2025 AT 19:29 PMMy mom had a rash on amoxicillin when she was pregnant with me. We all assumed she was allergic. Turned out it was just a viral rash. She got tested last year-negative. Now she takes penicillin for every infection. It’s crazy how much we just accept labels without ever checking if they’re real.
Carolyn Woodard
December 8, 2025 AT 01:42 AMThe immunological mechanisms underlying immediate hypersensitivity reactions to beta-lactams involve IgE-mediated degranulation of mast cells and basophils, which can be effectively probed via standardized skin prick and intradermal testing with major and minor determinant antigens. The negative predictive value approaches 98% in penicillin-allergy workups, making it a highly reliable tool for de-labeling. However, the absence of validated reagents for non-beta-lactam agents like NSAIDs and fluoroquinolones limits clinical utility in those domains, necessitating graded challenges as a complementary diagnostic modality.
Allan maniero
December 8, 2025 AT 21:07 PMI’ve been an ER nurse for 22 years. I’ve seen people get C. diff because they were given clindamycin instead of penicillin because of a false allergy label. I’ve seen kids with pneumonia get IV vancomycin when amoxicillin would’ve cleared it in 48 hours. This isn’t just about convenience-it’s about saving lives and cutting costs. If your doctor won’t refer you for testing, find one who will. You’re not being paranoid-you’re being smart.
Anthony Breakspear
December 9, 2025 AT 10:28 AMLet me tell you-this is the kind of thing that changes your life. My buddy got tested after avoiding penicillin since he was 5. Turned out he wasn’t allergic. He took amoxicillin for a tooth infection, saved $800 on antibiotics, didn’t get sick from the stronger stuff, and didn’t have to take 12 pills a day. Now he’s telling everyone. This isn’t just science-it’s freedom.
Zoe Bray
December 9, 2025 AT 15:39 PMIt is imperative that clinical decision-making regarding drug allergy status be grounded in evidence-based diagnostic protocols, including standardized skin testing methodologies and, where appropriate, supervised oral challenges. The persistence of unsubstantiated allergy labels contributes significantly to antimicrobial stewardship challenges and increased healthcare expenditures. A multidisciplinary approach involving allergists, infectious disease specialists, and primary care providers is essential for systematic de-labeling initiatives.
william tao
December 11, 2025 AT 00:27 AMSo… let me get this straight. You want me to trust a needle test from a doctor who couldn’t diagnose a cold without a $500 scan? And you think I’m supposed to just ‘try’ the drug again? What if it kills me? What if it’s not the drug, but the hospital air? Or the water? Or the government’s secret additives? I’ll keep avoiding it. Thanks, but no thanks.
Sandi Allen
December 12, 2025 AT 16:48 PMWait-so you’re telling me… the same people who told me I’m allergic… are now telling me I’m NOT allergic? And I’m supposed to believe them? What if they changed their minds because they’re paid by Big Pharma? And what if the ‘negative’ result is just a placebo? And what if the test causes a delayed reaction? And what if the ‘standardized’ kits are fake? And what if… I’m being manipulated?!