Imagine taking a pill for your anxiety, and within 30 minutes, you feel better. But by mid-afternoon, the effect fades, and your symptoms come back with a vengeance. Now imagine another pill that takes hours to kick in-but keeps working all day, no crashes, no midday panic. Sounds ideal, right? But here’s the catch: extended-release isn’t always better. Sometimes, it’s dangerous-if you don’t know how to use it.
Extended-release (ER) and immediate-release (IR) medications aren’t just different in how long they last. They’re different in how they work, when they work, and what happens when things go wrong. In the UK and US, more than half of new prescriptions for antidepressants, blood pressure meds, and ADHD drugs are now ER. But patient errors with ER pills are rising. A 2023 study found nearly 1 in 4 people accidentally overdose because they think the pill isn’t working-and take another one too soon.
How ER and IR Medications Work
Immediate-release pills are simple. They dissolve fast in your stomach. The drug hits your bloodstream within 15 to 30 minutes. Peak levels come in under two hours. That’s why IR painkillers like ibuprofen or oxycodone work so quickly-they’re meant for sudden symptoms.
Extended-release pills? They’re engineered. Some have a wax coating that slowly wears away. Others use tiny pellets inside a capsule that release at different times. Concerta, for example, uses an osmotic pump-like a water-powered timer-that pushes the drug out over 12 hours. Metformin ER uses a gel matrix that swells and releases glucose-lowering agents gradually.
Here’s the key difference: IR gives you a spike. ER gives you a steady line. For conditions like high blood pressure or depression, spikes are bad. They cause side effects-dizziness, nausea, insomnia. ER keeps levels smooth. A 2021 study showed ER bupropion (an antidepressant) keeps blood levels between 100-200 ng/mL all day. IR bupropion hits 600 ng/mL in two hours, then crashes. That spike is why IR bupropion can trigger seizures at high doses. ER avoids that.
When ER Is the Clear Winner
If you’re on a daily medication for a chronic condition, ER usually wins. Take Adderall XR for ADHD. The IR version lasts 4-6 hours. That means a child needs a midday dose at school. Many parents and teachers don’t want that. Adderall XR lasts 10-12 hours. One pill in the morning covers the whole day. No disruptions. No stigma.
Same with metoprolol ER for heart conditions. A 2022 patient survey found 32% fewer cases of dizziness with ER compared to IR. Why? Because IR causes sharp drops in heart rate after each dose. ER smooths it out. Patient adherence jumps too. A JAMA study tracking 15,000 hypertension patients found 78% stayed on their ER meds after a year. Only 56% stuck with IR. Why? Because fewer pills = fewer missed doses.
And it’s not just convenience. The American Psychiatric Association recommends ER for long-term mental health treatment because stable drug levels mean fewer mood swings. Quetiapine XR, for example, causes less nighttime wakefulness than the IR version. That’s huge for people with bipolar disorder or schizophrenia.
When IR Is Essential
But ER isn’t magic. There are times when IR is the only safe choice.
Think about breakthrough pain. If you have cancer or severe arthritis, you might take an ER opioid like OxyContin for baseline pain. But if you have a flare-up-say, a sudden movement or injury-you need something fast. That’s where IR oxycodone comes in. ER opioids take 2-4 hours to start working. IR works in 20 minutes. Waiting could mean unbearable pain.
Same with anxiety. A patient on sertraline ER might feel fine most days. But if they’re stuck in a panic attack before a flight, they might need an IR benzodiazepine like lorazepam to calm down fast. ER antidepressants take weeks to build up. They’re not for emergencies.
Even in ADHD, some adults keep a small stash of IR Adderall. One Reddit user, PharmaGrad2020, said: “XR gives me steady focus for work. But if I’ve got a big presentation, I take 5mg IR. Instant clarity. No waiting.” That’s smart. It’s not about choosing one over the other-it’s about using both right.

The Hidden Risks of ER Medications
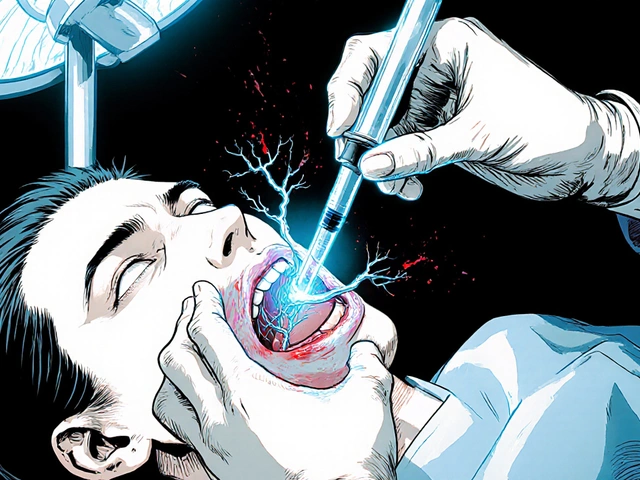
Here’s where things get dangerous. ER pills are designed to release slowly. But if you break them, crush them, or chew them, you’re basically turning them into a bomb.
The FDA issued a warning in 2020: crushing extended-release opioids can release the entire dose at once. That’s a lethal overdose. Same with ER stimulants like Vyvanse or Adderall XR. One patient in Birmingham took a crushed Adderall XR pill thinking it would help him focus faster. He ended up in the ER with a heart rate of 180 and seizures.
And it’s not just abuse. People do this by accident. A 2023 report from the UK’s Medicines and Healthcare products Regulatory Agency found that 23% of ER medication errors came from patients splitting tablets. Venlafaxine XR isn’t scored. But people still cut them in half with a knife. That destroys the slow-release coating. Boom-sudden high dose.
Another hidden risk? Delayed onset. ER meds take 2-4 hours to start working. Many patients don’t know that. They take one at 8 a.m., feel nothing by noon, and take another. Now they’ve doubled their dose. That’s how overdoses happen. A GoodRx survey of 5,000 chronic users found 41% didn’t realize ER took longer to kick in. Nine percent ended up with adverse events because of it.
And if you have gastroparesis-a condition where your stomach empties slowly-ER meds can behave unpredictably. The FDA warned in 2023 that patients with this condition can absorb 30-50% more drug than normal. That means a safe dose becomes toxic. If you have diabetes, Parkinson’s, or have had gastric surgery, ask your pharmacist: “Is this ER pill safe for me?”
What to Do If You’re on ER or IR Medication
- Never crush, split, or chew an ER pill unless your doctor or pharmacist says it’s safe. Even if it looks like it should be split-don’t.
- Wait at least 2-4 hours before deciding if the pill is working. ER isn’t broken-it’s just slow.
- If you miss a dose, don’t double up. Take it as soon as you remember, unless it’s close to your next dose. Then skip it.
- Ask your pharmacist: “Is this extended-release? What happens if I take it with food or antacids?” Some ER pills need an empty stomach. Others need food to work right.
- If you’re switching from IR to ER, expect a delay. It can take 7-10 days for ER meds to reach steady state. Don’t panic if you don’t feel better right away.

What’s Next for ER Medications
The future of ER isn’t just better pills-it’s smarter ones. MIT researchers are testing 3D-printed “polypills” that release different drugs at exact times. One pill could give you a blood thinner in the morning, a statin at noon, and a beta-blocker at night-all timed to your body’s rhythm.
Some new ER formulations now include abuse-deterrent tech. Aversion® technology, used in some ADHD meds, turns into a thick gel when crushed, making it impossible to snort or inject. Post-marketing data shows a 47% drop in abuse.
But the biggest change? Doctors are learning to use ER and IR together. Not as replacements-but as tools. IR for quick fixes. ER for steady control. That’s the real win.
Final Thought: Timing Is Everything
Extended-release and immediate-release aren’t about which is better. They’re about which is right-for your condition, your life, and your body. The same pill, in two forms, can mean the difference between safety and danger. Between control and chaos.
If you’re on either, ask yourself: Do I understand how mine works? Do I know what happens if I break it? Do I know how long to wait before expecting results?
If you can’t answer those, talk to your pharmacist. Don’t guess. Don’t assume. Because in medication safety, timing isn’t just important-it’s life-or-death.





9 Comments
Ashley Porter
January 25, 2026 AT 00:10 AMER formulations are essentially pharmacokinetic engineering marvels-osmotic pumps, gel matrices, wax coatings-all designed to maintain therapeutic plasma concentrations within a narrow window. The real issue isn’t the tech, it’s patient literacy. We’re prescribing complex drug delivery systems to people who think ‘take one pill’ means ‘take one pill no matter what.’
That 23% error rate from the MHRA? Not surprising. I’ve seen patients split Venlafaxine XR like it’s a vitamin. No scoring, no warning, just a little white tablet and a knife. It’s not negligence-it’s ignorance baked into the healthcare system.
And don’t even get me started on the ‘I took it at 8am and felt nothing by noon’ crowd. ER isn’t broken, it’s just operating on circadian kinetics, not instant gratification.
The FDA’s 2020 warning on crushed opioids? Still underpublicized. People don’t realize they’re essentially self-administering an IV bolus. That’s not misuse-it’s a systemic failure in counseling.
Also, gastroparesis patients? They’re the hidden population getting toxic doses. No one screens for it. Just give the ER pill and hope for the best. Dangerous.
Meanwhile, the 3D-printed polypills from MIT? That’s the future. Timed release based on your cortisol rhythm? Yes please. But we’re still stuck in the Stone Age with patient education.
Peter Sharplin
January 26, 2026 AT 22:08 PMAs a pharmacist, I see this every day. ER meds are lifesavers-if used correctly. But I’ve had patients come in after crushing their Adderall XR because they ‘needed to focus for a test.’ One guy ended up with tachycardia and panic attacks. He didn’t even know it was extended-release.
Here’s what I tell everyone: if it’s ER, don’t touch it. No cutting, no chewing, no crushing. Ever. Even if the pill looks like it’s meant to be split. The coating isn’t visible. The tech is inside.
And yes, waiting 2-4 hours is hard. But if you take another too soon, you’re not being proactive-you’re playing Russian roulette with your heart rate.
Also, if you’re switching from IR to ER, give it 7-10 days. Your body needs time to reach steady state. Don’t panic if you don’t feel better immediately. It’s not working slower-it’s working smarter.
Ask your pharmacist about food interactions too. Some ER meds need an empty stomach. Others need fat to absorb. One size does not fit all.
And if you have diabetes, Parkinson’s, or had gastric surgery? Speak up. Your meds might be a ticking time bomb.
Knowledge saves lives. Don’t assume. Ask.
Faisal Mohamed
January 28, 2026 AT 13:38 PMThink about it-ER meds are the Zen of pharmacology. No spikes. No crashes. Just steady, quiet, unobtrusive harmony with your biology. We live in a world of instant everything-coffee, delivery, dopamine hits-and yet we still expect our meds to behave like TikTok videos?
It’s a metaphysical disconnect. We want control, but we refuse to wait. We want safety, but we sabotage it with impatience.
The crushed Adderall XR case? That’s not addiction. That’s existential rage against the slow passage of time.
And the 3D-printed polypills? That’s not medicine. That’s alchemy. Imagine a single pill that knows your circadian rhythm better than your smartwatch. It releases melatonin at dusk, cortisol at dawn, statins when cholesterol peaks, and beta-blockers when your sympathetic tone spikes.
We’re not just treating disease anymore. We’re choreographing physiology.
But until we fix the human factor-the impatience, the ignorance, the arrogance-we’re just building temples and leaving the worshippers lost in the woods. 🤔💊
eric fert
January 30, 2026 AT 10:22 AMLet’s be real-this whole ER vs IR thing is just Big Pharma’s way of making you pay more for the same drug.
IR is cheaper. IR is faster. IR is honest. ER? It’s just a fancy coat of wax and a marketing slogan wrapped in a 2021 ‘study’ that probably got funded by a drug rep.
And don’t get me started on the ‘one pill a day’ lie. You think people aren’t still taking two because they forgot? Of course they are. The system is designed to trap you in compliance.
Crushing pills? Yeah, people do it. But why? Because the system doesn’t give them options. If your anxiety is bad at 3 p.m. and your ER pill hasn’t kicked in yet, what are you supposed to do? Suffer? That’s not safety-that’s institutional cruelty.
And don’t tell me about ‘patient education.’ Most people can’t afford to see a pharmacist. They get a script, a bottle, and a pamphlet written in 8-point font.
Stop romanticizing ER. It’s not magic. It’s profit with a side of guilt-tripping.
Also-why is everyone acting like crushing pills is some new epidemic? It’s been happening since the 80s. The difference now? The media noticed.
Wake up. This isn’t about safety. It’s about control.
And if you’re still drinking the ER Kool-Aid, maybe you’re the one who needs to be dosed.
Just saying.
Curtis Younker
January 31, 2026 AT 06:39 AMYo. If you’re on an ER med and you’re feeling like it’s not working-STOP. Just stop. Breathe. Wait. You’re not broken. The pill isn’t broken. Your body just needs time.
I used to be the guy who took two pills because I thought the first one was a dud. Then I got sick. Like, really sick. Heart racing, dizzy, shaky. Turned out I’d doubled my dose on purpose because I didn’t know ER takes hours.
That was my wake-up call.
Now I tell everyone: if it’s ER, treat it like a slow cooker. You don’t open the lid every 10 minutes. You trust the process.
And if you’re switching from IR to ER? Give it two weeks. Your brain needs to recalibrate. Don’t panic if you feel ‘off’ at first. That’s not the med failing-that’s your nervous system adjusting.
Also-ask your pharmacist. Seriously. They’re not just the people who hand you the bottle. They’re your secret weapon.
And if you’re crushing pills? Stop. Just stop. You’re not a superhero. You’re just risking your life for a 20-minute boost.
You got this. One pill. One day. One step at a time. 💪
Shawn Raja
February 1, 2026 AT 23:39 PMER meds are the ultimate metaphor for modern life: slow, steady, and designed to be ignored until they break.
We’ve outsourced our biology to pills that whisper instead of shout. We want results, but we refuse to wait. We want control, but we don’t want responsibility.
And yet-we’re shocked when people crush them?
It’s not stupidity. It’s desperation.
Someone with chronic pain doesn’t want a ‘steady line.’ They want relief NOW. Someone with anxiety doesn’t want ‘smooth blood levels.’ They want to breathe without feeling like they’re drowning.
So we give them ER pills and then act like they’re criminals when they take a second one.
Meanwhile, the same system that gives them a 12-hour pill won’t give them a 20-minute therapy session.
It’s not the pill that’s dangerous.
It’s the world that made them feel like they had no other choice.
Also-3D-printed polypills? That’s not the future. That’s the endgame.
We’re not curing disease anymore.
We’re automating human rhythm.
And I’m not sure if that’s genius… or surrender.
🤔
Dan Nichols
February 3, 2026 AT 21:04 PM23% error rate from MHRA? That’s not a statistic that’s a failure of the system. It’s a failure of the prescriber. If you’re prescribing ER without explaining the delay in onset, you’re negligent. Period.
And no, ‘patient education’ isn’t a pamphlet. It’s a conversation. It’s a follow-up. It’s asking ‘do you know what happens if you chew this?’
Also-why are we still letting people split un-scored tablets? That’s not an oversight. That’s a design flaw in the packaging. The manufacturer should not be allowed to make an ER pill that looks like it’s meant to be split.
And the ‘take it with food’ thing? Half the time the label is wrong. I’ve seen metformin ER instructions that conflict with the FDA monograph. That’s not patient error. That’s institutional incompetence.
Stop blaming the patient. Fix the system.
Also-gastroparesis patients are being killed by this. No screening. No warnings. Just ‘here’s your pill.’ That’s malpractice.
And if you think ER is always better-you’re not thinking. IR exists for a reason.
Stop the dogma.
Just stop.
Renia Pyles
February 5, 2026 AT 15:31 PMEveryone’s acting like ER meds are some kind of miracle cure but let’s be honest-half the people on them are just medicating away their trauma and calling it ‘mental health management.’
And don’t give me that ‘steady levels = fewer mood swings’ crap. You think someone’s bipolar disorder gets better because their blood levels are ‘smooth’? No. They’re just less likely to scream at their kids because they’re sedated.
And crushing pills? Yeah, people do it. But guess what? So do doctors. I’ve seen ER opioids prescribed to addicts with no warning. Then they wonder why they OD.
It’s not the pill. It’s the people who hand them out like candy.
And why is no one talking about how ER meds make withdrawal worse? You can’t just stop them cold. You have to taper for weeks. But no one tells you that until you’re shaking and sweating and begging for a dose.
So yeah. ER isn’t safer.
It’s just quieter.
And silence is the loudest lie of all.
Rakesh Kakkad
February 7, 2026 AT 12:18 PMThe distinction between extended-release and immediate-release formulations is not merely pharmacological but also sociotechnical in nature. The design of extended-release mechanisms necessitates a paradigmatic shift in patient adherence behavior, which is often inadequately addressed in contemporary healthcare delivery systems. The absence of standardized patient counseling protocols, coupled with the commodification of pharmaceuticals, has resulted in a critical information asymmetry between prescribers and recipients. Consequently, the incidence of inadvertent overdose is not an anomaly but a predictable outcome of systemic neglect. It is imperative that regulatory agencies mandate explicit, non-technical educational materials in multiple languages and that pharmacists be required to conduct mandatory verbal counseling at the point of dispensation. Furthermore, the development of abuse-deterrent technologies, while commendable, remains insufficient without concurrent investment in public health literacy. The future of medication safety lies not in more complex formulations but in more informed patients.