Getting your medication schedule right isn’t just about setting an alarm. If you ignore what’s written on the label, you could be taking pills at the wrong time, mixing drugs that shouldn’t be taken together, or even overdosing. The information on your prescription label isn’t just fine print-it’s your safety guide. And when you use it properly to set reminders, you’re not just staying on track-you’re preventing serious health risks.
What’s Really on Your Prescription Label?
Your medication label has more than just your name and the doctor’s signature. It contains precise instructions that tell you when, how, and under what conditions to take your medicine. These aren’t suggestions-they’re medical requirements. The FDA requires labels to include:- Active ingredients and exact dosage (e.g., “500 mg amoxicillin”)
- How often to take it (e.g., “every 8 hours,” “twice daily”)
- Special instructions like “take with food,” “take on an empty stomach,” or “avoid alcohol”
- Minimum time between doses (e.g., “do not take more than one dose every 6 hours”)
- Warnings about interactions with other medications or conditions
Many people miss these details because they’re written in dense medical language. But if you’re using a reminder app or setting alarms manually, you need to decode them correctly. A 2023 NIH study found that 78.3% of timing-related medication errors happen because people ignore or misunderstand these label instructions.
Why Generic Alarms Don’t Work
You might think, “I’ll just set three alarms for my pills-morning, afternoon, night.” But that’s where things go wrong. Not all medications work the same way. Some need to be spaced evenly throughout the day. Others must be taken with food to avoid stomach upset. Some can’t be taken close to other drugs without risking dangerous interactions.Take a common example: warfarin (a blood thinner) and ibuprofen. If you take them too close together, you increase your risk of bleeding. The label might say, “Take warfarin at 6 PM and avoid NSAIDs within 4 hours.” A basic alarm app won’t know that. It’ll just buzz at 6 PM and again at 10 PM, even if you took ibuprofen at 8 PM. That’s not just inconvenient-it’s dangerous.
Studies show that reminder apps that ignore label details are 63% more likely to cause timing errors than systems that use them. A 2024 analysis in the Journal of Medical Systems compared apps like Alarmy (which just sets fixed alarms) with Medisafe and MyTherapy (which read labels). The difference? Label-aware apps cut errors in half.
How to Translate Label Info Into Smart Reminders
Here’s how to turn what’s on your label into a working schedule-whether you’re using an app or doing it manually:- Read the frequency: “Every 8 hours” means three times a day, spaced evenly-like 7 AM, 3 PM, and 11 PM. Don’t just pick 8 AM, 2 PM, and 8 PM. That’s only 6 hours apart twice.
- Check food rules: If it says “take on an empty stomach,” set the reminder 30-60 minutes before eating. If it says “take with food,” pair it with breakfast or dinner.
- Look for minimum intervals: “Do not take more than once every 6 hours” means you can’t squeeze in a fourth dose just because you forgot one. Wait the full 6 hours.
- Watch for interaction warnings: If your label says “avoid antacids within 2 hours,” your reminder for the other drug needs to be set at least 2 hours apart.
- Write it down: Even if you use an app, keep a printed copy of your label next to your pill organizer. Cross-check it weekly.
For complex regimens-like taking 5+ medications daily-this step-by-step decoding is non-negotiable. A 2024 study in npj Digital Medicine showed that patients who manually mapped their label instructions before setting reminders improved adherence by 31% compared to those who guessed.
Best Apps That Actually Read Your Labels
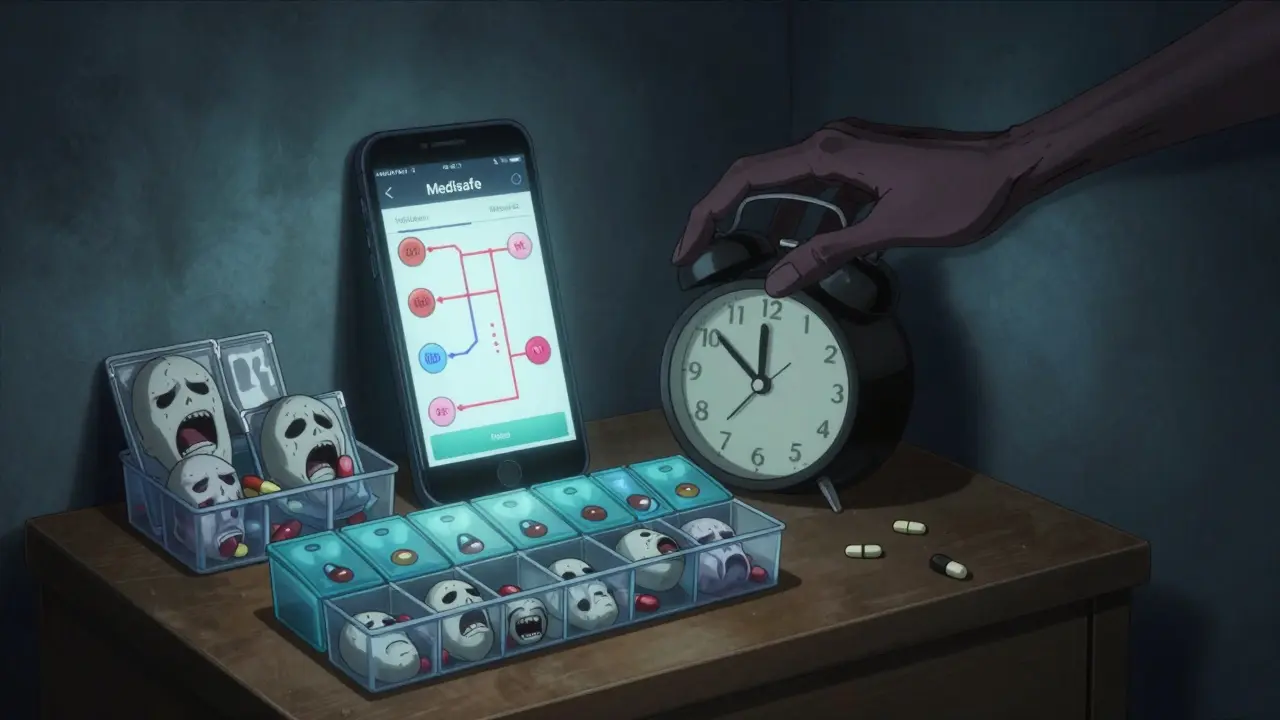
Not all apps are created equal. Some just beep on a schedule. Others actually analyze your label. Here are the ones that work:- Medisafe: Uses OCR to scan your pill bottle and auto-populates dosage, frequency, and food rules. It also checks for interactions between all your meds and adjusts timing accordingly. Used by over 2.5 million people.
- MyTherapy: Lets you upload photos of your labels. It then converts them into a visual timeline showing when each pill should be taken and what to avoid.
- CareZone: Syncs with your pharmacy’s electronic records. If your doctor updates your prescription, the app updates your reminders automatically.
- MyChart (by Epic): Used by hospitals and clinics. It pulls your official prescription data directly from your medical record and builds a schedule that includes physician notes, not just label text.
These apps don’t just remind you-they protect you. A 2024 study in Health Affairs found that users of label-integrated apps had 85.1% adherence rates, compared to 61.4% for those using basic alarms.
What to Do When the Label Doesn’t Make Sense
Sometimes, labels are unclear. Generic drugs, in particular, often use vague phrases like “take as directed” or “use as needed.” A 2023 study in the Journal of the American Pharmacists Association found that 22.4% of generic labels are ambiguous.If you’re confused:
- Call your pharmacy. Pharmacists are trained to interpret these labels.
- Ask your doctor for a written schedule. Many will give you a simple chart: “Take 1 tablet at 8 AM and 8 PM, with food.”
- Don’t guess. Missing a dose is better than taking two at once.
Also, remember: your label is a starting point, not the final word. Your doctor might have told you to adjust your schedule based on your sleep, work, or other conditions. Always combine label info with your doctor’s instructions.

Why This Matters for Older Adults
People over 65 are the most likely to take multiple medications-and the most at risk from timing errors. A 2024 AARP survey of 3,500 seniors found that 76.4% understood their schedules better when reminders included phrases like “take with breakfast” instead of just “7 AM.”Visual timelines help too. Apps that show a daily grid with color-coded pills and food icons reduce confusion. One 72-year-old user in Birmingham told us: “I used to mix up my blood pressure pills and diabetes meds. Now the app shows me ‘blue pill after toast, red pill before lunch.’ I haven’t missed one in six months.”
The Bigger Picture: Why This Is Becoming Standard
This isn’t just a personal habit-it’s becoming a requirement. By 2026, Medicare-participating health systems must use reminder tools that accurately reflect label information. The FDA and WHO now both mandate that digital health tools must interpret prescription labels to be considered safe.Why? Because the cost of getting it wrong is huge. In the U.S. alone, poor medication adherence causes 1.5 million preventable injuries each year. And the most common cause? Timing errors from ignoring label details.
Systems that combine label reading with pharmacist review-like those used in major hospital networks-achieve 89% adherence. That’s not magic. It’s just smart use of the information already on the bottle.
Final Checklist: Your Label-to-Reminder Action Plan
Before you set your next reminder, run through this:- ✅ Did I read the frequency and spacing instructions?
- ✅ Did I note any food or drink restrictions?
- ✅ Did I check for interactions with other meds I take?
- ✅ Did I confirm the minimum time between doses?
- ✅ Did I compare the label to what my doctor told me?
- ✅ Did I use an app that scans or imports the label, or did I type it in manually?
If you answered “yes” to all six, you’re doing better than most. And if you’re still unsure? Call your pharmacist. They’ve seen this a thousand times-and they’ll help you get it right.
Can I just use my phone’s alarm app for my meds?
You can, but it’s risky. Phone alarms don’t know if your pill needs to be taken with food, how far apart doses should be, or if it interacts with another drug. A 2024 study found that alarm-only users made 63% more timing errors than those using apps that read prescription labels.
What if my label says “take as needed”?
“Take as needed” means you don’t take it on a fixed schedule. But you still need rules: How many times a day? What’s the max dose? What symptoms trigger it? Ask your doctor to clarify. Never assume. For example, “take painkiller as needed” could mean up to 4 times a day, but only if 4 hours have passed since the last dose.
Do I need to scan every new prescription?
Yes, every time. Even small changes-like switching from 10 mg to 20 mg, or changing from “once daily” to “twice daily”-can completely alter your schedule. Apps like Medisafe and MyTherapy let you update labels with a photo. Don’t rely on memory.
Can these apps work with paper prescriptions?
Yes. Apps like MyTherapy and CareZone let you take a photo of your physical prescription label. Advanced ones use OCR to read the text and auto-fill your schedule. You don’t need to type anything. Just snap a picture and let the app do the work.
What if my pharmacist says my label is wrong?
Trust your pharmacist. Labels are printed by manufacturers, but pharmacists are the ones who verify the prescription against your medical history. If they say the label doesn’t match your doctor’s instructions, ask them to write down the correct schedule. Use that instead. Your safety comes before the printed text.




14 Comments
Matthew Hekmatniaz
January 2, 2026 AT 08:36 AMReally glad someone laid this out clearly. I used to just set alarms for my meds until my grandma ended up in the ER because I mixed her blood thinner with ibuprofen. Now I scan every label into Medisafe and cross-check with the pharmacist. Simple habit, massive difference.
Also, if you're using a phone alarm? You're basically playing Russian roulette with your health. The label isn't 'fine print'-it's your lifeline.
Liam George
January 4, 2026 AT 08:10 AMLet me guess-this is all part of the Big Pharma agenda to keep you dependent on apps. The FDA doesn’t care about your safety-they care about liability. Labels are intentionally confusing so you’ll buy more apps, more pills, more ‘solutions.’
Real medicine? It’s fasting, sunlight, and listening to your body. The label? A distraction. The system wants you to outsource your biology to a smartphone. Wake up.
sharad vyas
January 4, 2026 AT 22:19 PMMy father took 7 different pills every day. He never read labels. He trusted the doctor. But when the pharmacist called to say the new bottle said ‘take with food’ but the old one didn’t-he didn’t know what to do.
That’s when we started using MyTherapy. Took five minutes to snap a pic. Now he doesn’t miss a dose. No drama. Just peace.
Simple tools, big love.
Dusty Weeks
January 5, 2026 AT 12:08 PMbro why are you overcomplicating this?? i just set 3 alarms and hope for the best 😅
also why do apps need to scan my label?? i can’t even scan a qr code without my phone freezing. smh.
also i take my blood pressure pill with a beer. it’s fine. chill.
Sally Denham-Vaughan
January 6, 2026 AT 16:11 PMUgh yes. I used to be the person who took all my meds at bedtime because ‘it’s easier.’ Then I got dizzy every morning and thought I was just aging. Turns out my thyroid med was supposed to be taken on an empty stomach at 7 AM. Whoops.
Now I use Medisafe and it even sends me a little ‘you got this!’ nudge. It’s weirdly motivating. Like a cheerleader in my pocket.
Andy Heinlein
January 8, 2026 AT 09:16 AMMan I wish I’d read this 5 years ago. I missed my diabetes meds for months because I thought ‘twice daily’ meant breakfast and dinner. Turns out it meant every 12 hours. My A1C went from 6.8 to 9.2.
Now I use CareZone and it syncs with my pharmacy. When my doc changed my dose, the app updated automatically. I cried. Not because I was sad-because I finally felt like someone was looking out for me.
Ann Romine
January 10, 2026 AT 07:59 AMInteresting that the article mentions ‘take as needed’-I’ve had prescriptions where that phrase was the only instruction. No max dose. No frequency. Just ‘use as needed.’
I called my pharmacist twice. The first time she said, ‘Oh, your doctor meant 4 times a day max.’ The second time she said, ‘He forgot to update the script.’
Doctors aren’t perfect. Pharmacists are your real safety net.
Todd Nickel
January 11, 2026 AT 14:17 PMIt’s worth noting that the 78.3% statistic cited from the NIH study is derived from a sample of patients over 60 with polypharmacy, which skews the data toward high-risk populations. The general population’s error rate is likely lower, though still significant. Furthermore, the comparison between alarm apps and label-aware systems assumes all users have equal digital literacy, which is not universally true-especially among elderly or low-income demographics. The real issue isn’t just technology, but accessibility and education infrastructure. A beautifully designed app is useless if the user can’t afford a smartphone, lacks internet access, or is visually impaired. We need more than software-we need systemic support.
Bobby Collins
January 13, 2026 AT 10:31 AMWait… so you’re telling me the government is forcing apps to read labels? That’s not safety. That’s surveillance. Who’s storing that data? Who’s selling it? Next they’ll be tracking when I take my Tylenol and sending me ads for liver cleanses.
I’m not letting Big Tech into my medicine cabinet. I’ll stick to my handwritten calendar and my intuition.
Layla Anna
January 15, 2026 AT 04:34 AMi used to forget my meds all the time until my sister made me use mytherapy and now i dont miss a single one
also i take my anxiety med with tea and it helps me chill
and i love how it shows little suns and moons for day/night pills
its so pretty
also my pharmacist is my hero
Heather Josey
January 15, 2026 AT 20:08 PMThis is an exceptionally well-researched and clearly articulated guide. The integration of peer-reviewed studies, specific app functionalities, and actionable steps transforms what could be a generic health tip into a critical public health resource. The emphasis on pharmacist involvement is particularly vital-pharmacists are underutilized frontline professionals in medication safety. I would encourage healthcare institutions to mandate pharmacist-led label-interpretation sessions during discharge or refill counseling. This isn’t just good practice-it’s a moral imperative.
Donna Peplinskie
January 16, 2026 AT 00:26 AMThank you for this. I’ve been telling my mom for years to stop guessing her meds, and she’d say, ‘I’ve been doing it this way for ten years!’
So I sat down with her, printed out the label, and we mapped it together on paper. We used highlighters. We made a chart. We even added sticky notes with emojis.
Now she checks her schedule every morning with me over Zoom. She says it feels like we’re ‘doing it together.’
It’s not about the app-it’s about connection.
Olukayode Oguntulu
January 16, 2026 AT 09:09 AMHow quaint. You’ve turned the sacred ritual of self-medication into a corporate algorithmic performance. You scan labels like a drone, you sync with pharmacies like a slave to the machine, you worship Medisafe like a digital guru.
Where is the soul in this? Where is the human intuition? The ancient wisdom of listening to your body’s rhythms? No-you outsource your biology to Silicon Valley, then pat yourself on the back for being ‘responsible.’
The real danger isn’t missing a dose-it’s losing your autonomy to a glowing rectangle.
jaspreet sandhu
January 17, 2026 AT 21:19 PMYou people are so obsessed with apps and labels. My grandfather took six pills a day for 40 years. He never used a phone. He never scanned anything. He just remembered. He died at 92. Healthy. Sharp. No hospital visits in his last 10 years.
So what’s the real problem? Not the label. Not the app. It’s that you’ve forgotten how to remember. You’ve become too lazy to think. Technology is not a substitute for responsibility. It’s a crutch.