When you’re told to take a pill every day for the rest of your life, the biggest question isn’t whether it works-it’s whether you can afford it. For millions of Americans, the price tag on their prescription decides whether they take it at all. And the data doesn’t lie: when generic drugs cost less, people actually take them. Not just a little more. A lot more.
Why Price Still Matters, Even When Generics Are Just as Good
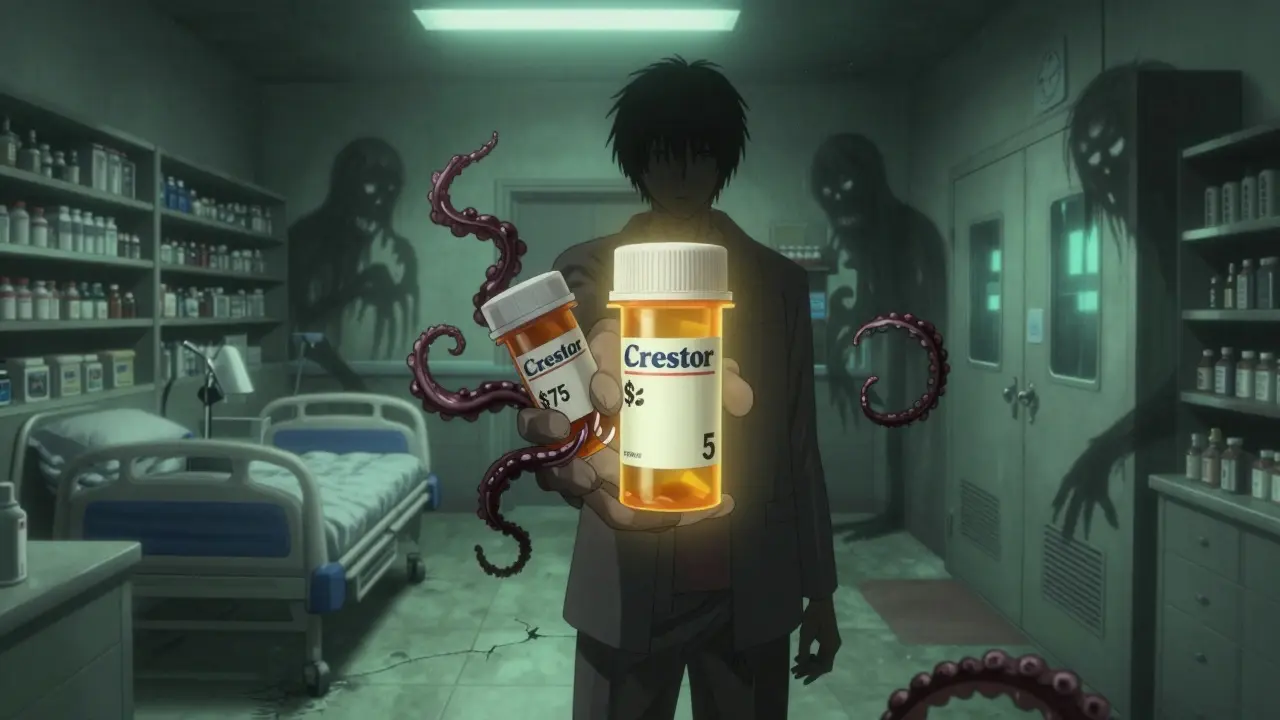
Generic drugs aren’t cheap because they’re low quality. They’re cheap because they don’t need to pay for marketing, clinical trials, or patent protection. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed in the body at the same rate and extent-within 80% to 125% of the brand. That’s not a guess. That’s science. Yet, even with this equivalence, patients still hesitate. Why? Because out-of-pocket costs add up fast. A brand-name statin like Crestor might cost $75 a month with insurance. The generic, rosuvastatin? $5. That’s not a price difference. That’s a life-changing gap. A 2012 study tracking Medicare Part D patients found that when doctors switched patients from brand-name statins to generics, adherence jumped by 5.9%. That’s not a small uptick. That’s thousands of people who stopped skipping doses, avoided hospital visits, and stayed out of emergency rooms. And it wasn’t just statins. For breast cancer patients on aromatase inhibitors, those on generics had 73.1% adherence compared to 68.4% for those on brand names. Higher copays? Higher dropout rates.The Dose-Response Effect: Every $10 Increase, Lower Adherence
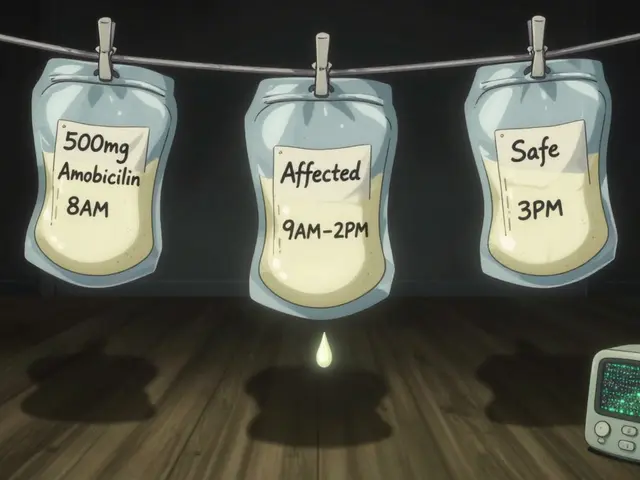
It’s not just big jumps that matter. Even small increases in cost have measurable effects. Research shows that for every $10 rise in out-of-pocket cost, adherence drops by 2% to 4%. That’s true across conditions-from diabetes to depression to high blood pressure. A 2023 study in Diabetes Care looked at GLP-1 receptor agonists, expensive drugs used for type 2 diabetes and weight loss. Every $10 increase in patient cost reduced the chance of adherence by 3.7%. And the ripple effect? A 5.2% increase in emergency room visits. That’s not just about pills. That’s about people ending up in the hospital because they couldn’t afford to stay healthy. The numbers are brutal. Medication nonadherence causes up to 50% of treatment failures. It leads to over 100,000 preventable deaths each year in the U.S. And it costs the system between $100 billion and $300 billion annually. That’s not just wasted money. That’s wasted time, pain, and lives.
Real People, Real Stories: When Generics Changed Everything
Behind every statistic is someone who skipped a dose because they had to choose between medicine and groceries. Or who filled their prescription once, then stopped because the next refill was too expensive. One Reddit user, u/HeartHealthJourney, shared their story in March 2024: “After my cardiologist switched me from brand-name Crestor ($75 copay) to generic rosuvastatin ($5 copay), I went from missing 3-4 doses weekly to perfect adherence for 11 months straight.” That’s not an outlier. A 2023 JAMA Network Open survey of over 2,100 adults found that 32.7% admitted to cost-related nonadherence-skipping doses, delaying refills, or not filling prescriptions at all to save money. And of those people, 78% said if they’d known the real price before starting the drug, they might not have taken it at all. Even more telling: 54% of people who skipped doses because of cost said they’d be “moderately or extremely upset” if their doctor used a price-checking tool but never mentioned the cost. They don’t want to be surprised. They want to be heard.How the System Is Starting to Fix Itself
The good news? Change is happening-and it’s working. The Inflation Reduction Act of 2022 capped insulin at $35 a month. That alone is saving lives. By 2025, Medicare Part D will have a $2,000 annual cap on out-of-pocket drug spending. That’s huge for seniors on multiple medications. Real-time benefit tools (RTBTs) are now being integrated into electronic health records. When a doctor writes a prescription, the system shows the patient’s exact out-of-pocket cost at their local pharmacy. In pilot programs, this simple change improved adherence by 12% to 15%. One pharmacy benefit manager, Magellan, reported a 40% reduction in care gaps and a 2:1 return on investment. The FDA’s “It’s Okay to Use Generics” campaign is helping too. Many patients still think generics are weaker. They’re not. But education matters. When pharmacists explain bioequivalence, adherence improves. When doctors say, “This generic works just as well and saves you $70 a month,” patients listen.




9 Comments
michelle Brownsea
January 21, 2026 AT 04:14 AMLet’s be brutally honest: if you can’t afford your medication, you’re not failing-you’re being failed by a system that treats health like a luxury subscription. Generics aren’t ‘cheaper alternatives’; they’re the only morally defensible option. The fact that we still debate this in 2025 is a national shame. And yes, I’m calling out every politician who takes pharma donations while seniors ration insulin. This isn’t policy. It’s cruelty dressed up as capitalism.
lokesh prasanth
January 22, 2026 AT 00:42 AMstats say yes but real life? people skip meds not just for cost but for forgetfulness, depression, or just plain dumb. generics dont fix human behavior. also why u always blame pharma? pharmacy benefit managers are the real villains.
Malvina Tomja
January 22, 2026 AT 02:44 AMOh please. Let’s not pretend this is about ‘affordability.’ It’s about entitlement. People expect miracle drugs at grocery-store prices. Meanwhile, I pay $12 for my generic lisinopril and I’m grateful. If you can’t afford $5 a month, maybe you should’ve budgeted better instead of blaming doctors and drug companies. Also, ‘bioequivalence’ isn’t a marketing slogan-it’s FDA science. Get informed.
Yuri Hyuga
January 22, 2026 AT 05:38 AMThis is the kind of post that gives me hope 🌱
Every time someone chooses a generic, they’re not just saving money-they’re choosing life. And when doctors use real-time pricing tools? That’s healthcare with heart. Let’s celebrate the pharmacists who explain bioequivalence. The nurses who check in. The systems that work. Change isn’t loud-it’s quiet, daily, and human. Keep pushing. We’re getting there. 💪❤️
MARILYN ONEILL
January 23, 2026 AT 05:35 AMOMG I can’t believe people still don’t get it. Generics are literally the same. Same pill. Same factory. Same everything. If you’re still taking brand-name Crestor because you ‘trust it more’-you’ve been scammed. And no, your ‘gut feeling’ doesn’t override clinical trials. Just stop. Please.
Steve Hesketh
January 24, 2026 AT 04:50 AMI come from a village where medicine was once a prayer and a shared bowl of soup. Now, here in the U.S., we have the best science on earth-but we make people choose between pills and rent. This isn’t just a policy issue. It’s a soul issue.
When my cousin skipped her diabetes meds because the copay doubled? She ended up in the ER. Not because she was lazy. Because she was poor. And that’s not a medical problem. That’s a moral failure. We can do better. We must.
Sangeeta Isaac
January 25, 2026 AT 18:02 PMso like… i got my generic metformin for $3 at walmarts pharmacy and i was like… wait… i could’ve been doing this for 3 years?? 😳
my doctor never mentioned it. my insurance never told me. i just… assumed it was expensive. turns out i was just bad at googling. also why do i feel guilty for saving $70/month? like… is that weird? 🤔
Alex Carletti Gouvea
January 26, 2026 AT 06:58 AMGenerics? That’s just socialism in pill form. If you want cheap medicine, move to Canada. We built a world-class pharmaceutical industry here-don’t punish innovation because some people can’t budget. The free market works. People just need to work harder.
Philip Williams
January 27, 2026 AT 02:21 AMWhile the data on adherence and cost is compelling, one critical variable remains underexamined: the role of health literacy. A patient may be able to afford a generic, but if they do not understand its equivalence, adherence remains compromised. Educational interventions-particularly those co-designed with patients-must be scaled alongside price reforms. The synergy of affordability and understanding is the true lever for systemic change.