When your insurance company denies your brand-name medication because a generic is available, but that generic makes you feel worse-or doesn’t work at all-you’re not just being stubborn. You’re dealing with a real medical problem that insurers often ignore.
Generic drugs are supposed to be the same as brand-name ones. The FDA says they must deliver 80% to 125% of the active ingredient. Sounds fair, right? But for some people, that 45% window isn’t just a technicality-it’s the difference between feeling stable and having a seizure, a thyroid crash, or a mental health spiral. That’s not theory. It’s happening to tens of thousands of patients every year.
Why Generics Sometimes Don’t Work
It’s not about quality. It’s about chemistry. Generics have the same active ingredient, but they use different fillers, dyes, and binders. For most people, that doesn’t matter. But for those on narrow-therapeutic-index drugs-like levothyroxine for thyroid disease, warfarin for blood clots, or levetiracetam for epilepsy-even tiny changes in how the drug is absorbed can throw off their entire treatment.
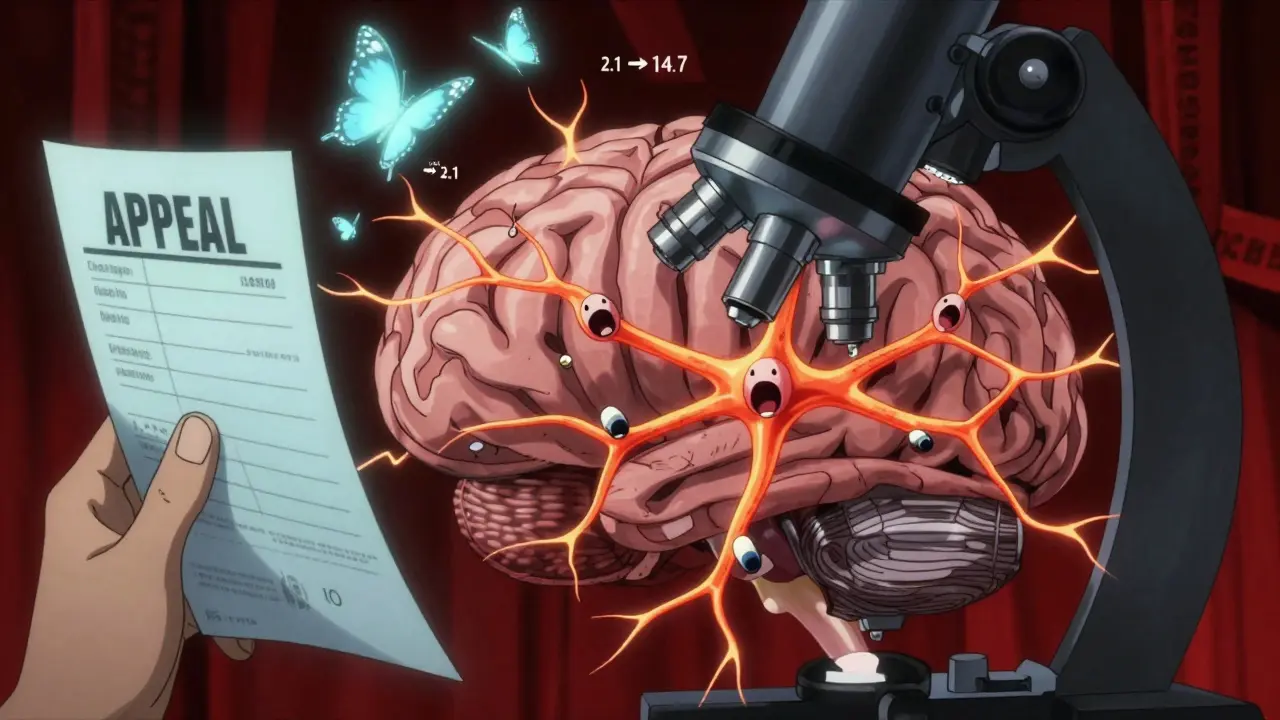
Take thyroid medication. One patient’s TSH level jumped from 2.1 to 14.7 after switching to a generic levothyroxine. That’s not a fluke. It’s a medical emergency. The Endocrine Society has guidelines warning against automatic switching for thyroid patients. Yet insurers still push generics without checking.
Same with epilepsy. A 2022 study from the Epilepsy Foundation found that 78% of appeals for brand-name antiseizure drugs were approved when patients had documented breakthrough seizures on generics. That’s because the brain doesn’t care if the pill looks different-it cares if the drug hits the right concentration at the right time. And for some people, generics just don’t deliver.
How Insurance Denials Work
Your insurer says no because their formulary lists a cheaper generic. The denial code? Usually DA2000: “Generic available.” They don’t ask if it worked. They don’t check your history. They just assume bioequivalence equals clinical equivalence.
But here’s the truth: bioequivalence doesn’t mean the same effect for every person. A 2023 analysis of 12,487 appeals by the Patient Advocate Foundation found that 67% of denials were overturned when patients had solid documentation. That’s not luck. That’s proof that the system can work-if you know how to fight it.
Denials happen fast. You get a letter saying your brand-name drug is no longer covered. You call the pharmacy. They say, “Just take the generic.” You try it. You feel dizzy. Your anxiety spikes. Your seizures return. You go back to your doctor. They write a letter. You submit an appeal. Then you wait. And wait. And wait.
What You Need to Win Your Appeal
There’s one thing that separates successful appeals from failed ones: documentation. Not just a note from your doctor saying “I think this is better.” You need proof.
- Lab results showing your levels changed after switching (TSH, INR, drug concentration)
- Medication logs tracking symptoms before and after the switch
- Emergency room visits or hospitalizations tied to the generic
- A detailed letter from your doctor explaining why the brand is medically necessary
Doctors who include specific ICD-10 codes and measurable outcomes-like “TSH increased from 2.1 to 14.7 over 8 weeks”-have a 76% approval rate. Those who just write “patient prefers brand name”? Around 29%.
For drugs like Synthroid, cite the FDA’s own labeling that says brand-name levothyroxine is specifically indicated for thyroid replacement. That’s not opinion-that’s fact. And insurers can’t ignore it.
How the Appeals Process Works
The process is the same whether you’re on Medicare, Medicaid, or private insurance-but the timelines differ.
For commercial insurance: You have 180 days to file an internal appeal. The insurer has 30 days to respond. If they say no, you can request an external review by an independent third party. That takes another 30-45 days. The success rate? 67% when you have good documentation.
For Medicare Part D: You have 60 days to appeal. The first level is handled by your plan. If denied, you can go to an independent review organization. Then to the Office of Medicare Hearings and Appeals. Then to the Medicare Appeals Council. Each step takes weeks. But if you’re on a life-saving drug, you can request an expedited review-72 hours or less.
States matter too. California, New York, and Texas have stronger protections. If you live in one of the 28 states that ban step therapy for documented therapeutic failure, you can skip trying multiple generics. Just show proof it didn’t work.
Real Stories, Real Results
One Reddit user, u/ThyroidWarrior, posted a detailed appeal after their TSH levels spiked on generic levothyroxine. They included lab reports, a doctor’s letter citing the Endocrine Society guidelines, and a timeline of symptoms. Their appeal was approved in 21 days.
Another, u/PainPatient, was denied for brand-name gabapentin after three seizure breakthroughs. The insurer said, “No clinical evidence.” They didn’t look at the ER records. They didn’t read the neurologist’s notes. The appeal was denied. They had to go to a nonprofit for help.
That’s the problem. Most people give up after the first denial. But the data doesn’t lie: 42% of initial appeals are denied-but 67% of external reviews are approved when you have the right paperwork.
Tools and Help That Actually Work
You don’t have to do this alone.
GoodRx’s Appeal Assistant is used by over 147,000 people in 2023. It walks you through building a letter your doctor can sign in minutes. Users rate it 4.7 out of 5.
The Patient Advocate Foundation offers free case management. Call 1-800-532-5274. Their team handles the paperwork, contacts your insurer, and tracks deadlines. In their 2023 report, 92% of users said they got the medication they needed.
Specialty pharmacies like OptumRx and Accredo now have dedicated appeal teams. Patients who used their services had a 73% approval rate-compared to 51% for those who tried alone.
What’s Changing in 2026
The system is slowly adapting. In 2024, CMS mandated that insurers process appeals for anti-seizure drugs within 72 hours. That’s because too many people were having seizures while waiting.
The FDA is also considering new guidance that acknowledges individual differences in how generics work. That could mean future approvals based on personal response-not just lab averages.
Meanwhile, 19 states have passed “right to try brand” laws. If you’ve tried two generics and they failed, you’re legally entitled to the brand-name drug.
And insurers? They’re starting to notice. 76% of large employers now include therapeutic inequivalence exceptions in their pharmacy contracts. The problem? Only 38% of patients know this exists.
What to Do Right Now
If you’re being denied a brand-name drug because a generic was pushed on you:
- Get your Explanation of Benefits (EOB) from your insurer. Look for the denial code (DA2000, DA1200).
- Collect your lab results, symptom logs, and ER records.
- Call your doctor. Ask for a letter that includes specific data: dates, dosages, lab values, symptoms.
- Submit your appeal within the deadline. Don’t wait.
- If denied, request an external review. That’s where most wins happen.
- Use GoodRx or the Patient Advocate Foundation if you’re overwhelmed.
This isn’t about being picky. It’s about survival. For some people, the generic isn’t just less effective-it’s dangerous. And the system is built to let you fight back.
You have rights. You have data. You have time. Use it.
What if my doctor won’t write the appeal letter?
Many doctors are overwhelmed, but they’re legally required to support medically necessary care. Ask for a 15-minute appointment specifically to discuss your appeal. Bring your lab results and symptom log. If they still refuse, contact the Patient Advocate Foundation-they can help you draft a letter your doctor can sign. Some states even have laws requiring providers to assist with appeals.
How long does an insurance appeal take?
Internal appeals take 30 days for commercial insurance. External reviews take another 30-45 days. For Medicare, the first level takes 7 days. If you’re in a medical emergency-like seizures or unstable thyroid levels-you can request an expedited review. Insurers must respond in 72 hours.
Can I switch back to the brand-name drug if the generic doesn’t work?
Yes-but you can’t just ask. You have to appeal. Insurers won’t let you switch without proof. That’s why documentation is everything. If you’ve already tried the generic and had negative effects, you’re eligible for an exception. Use your medical records to prove it.
Are there states that protect patients better?
Yes. California, New York, and Texas have higher approval rates because they require insurers to consider therapeutic inequivalence. 28 states ban step therapy for documented failures. Check your state’s insurance department website for formulary exception rules. You might have more rights than you think.
What if I can’t afford the brand-name drug even if approved?
The Inflation Reduction Act eliminated cost-sharing for successful Medicare Part D appeals. For commercial insurance, many manufacturers offer patient assistance programs. Check the Partnership for Prescription Assistance or NeedyMeds.org. You might get the drug for free or at a steep discount.