Medication Storage: How to Keep Your Pills Safe, Effective, and Ready to Use
When you buy medicine, you’re not just paying for the drug—you’re paying for it to work when you need it. That’s why medication storage, the practice of keeping drugs in conditions that preserve their strength and safety. Also known as drug storage, it’s not just about keeping pills out of reach of kids—it’s about keeping them alive. Heat, moisture, and light can break down active ingredients faster than you think. A pill sitting on your bathroom counter might look fine, but if it’s been exposed to steam from your shower every day, it could be losing potency. The FDA doesn’t require expiration dates to be based on real-world storage, so what’s on the bottle? That’s just the manufacturer’s best guess under ideal conditions. Real life? It’s messier.
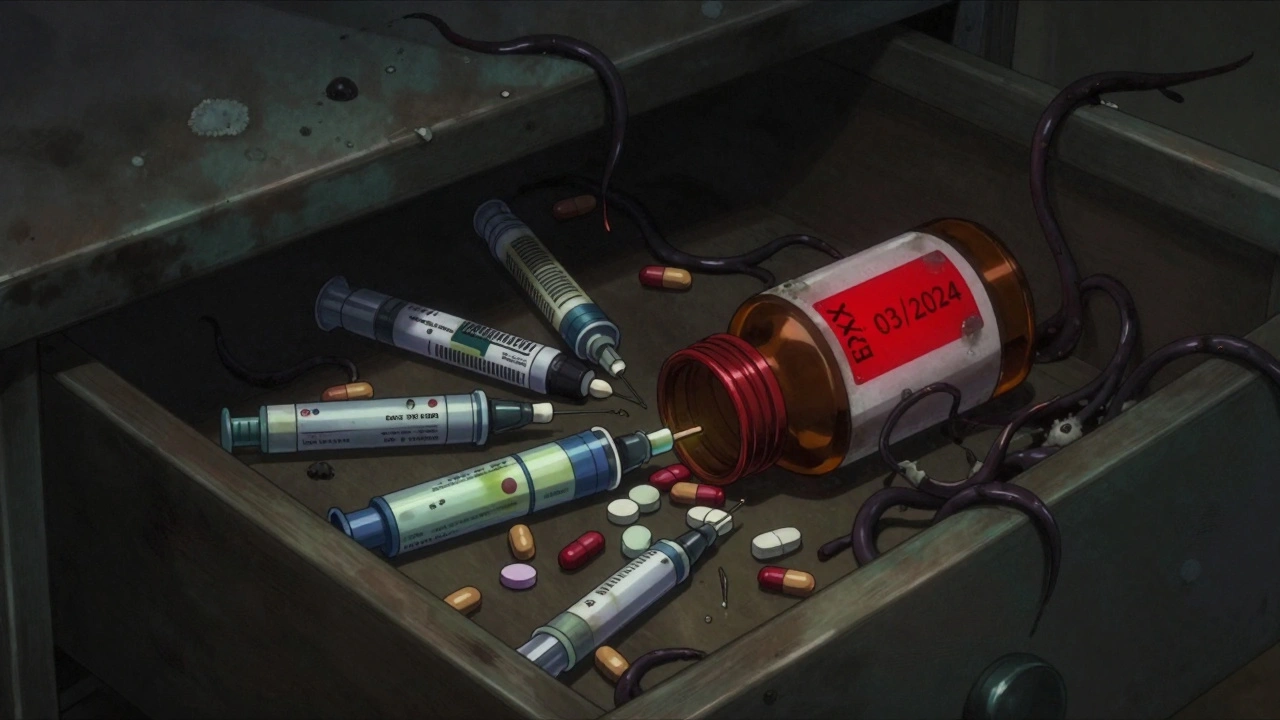
Medicine expiration, the point after which a drug’s effectiveness is no longer guaranteed. Also known as drug shelf life, it’s not a hard stop—some medications last years beyond their date if stored right. But others? They degrade fast. Insulin, for example, starts losing strength within weeks if left unrefrigerated. Antibiotics like amoxicillin can turn into toxic compounds when exposed to moisture. And don’t assume your medicine cabinet is safe. Most are warm, damp, and full of air changes from opening and closing. That’s why the best place for most pills? A cool, dry drawer—not the bathroom, not the kitchen near the stove, not the car glovebox. Temperature matters. Most drugs are stable between 68°F and 77°F. If it’s hot where you live, consider keeping your meds in the bedroom closet. Humidity? That’s the silent killer. Moisture causes tablets to crack, capsules to stick, and powders to clump. Silica gel packets? Keep them in the bottle. They’re there for a reason. And light? UV rays can break down certain drugs like birth control pills and thyroid meds. Amber bottles help, but if your meds came in clear plastic, store them in a dark box.
And then there’s the people who forget. The ones who leave their insulin on the counter for weeks. The ones who take old antibiotics from last year’s infection. The ones who keep their pain pills in the same drawer as their vitamins, their supplements, their kids’ chewables. Pill safety, the set of practices that prevent accidental poisoning, misuse, and ineffective treatment. Also known as drug safety, it’s not just about keeping kids away—it’s about keeping your own meds working as intended. A study in the Journal of the American Pharmacists Association found that over 30% of people store their meds in places that compromise their stability. And that’s not just about wasted money—it’s about your health. If your blood pressure pill loses strength, your risk of stroke goes up. If your seizure med degrades, you’re one seizure away from disaster.
You don’t need a climate-controlled vault. Just a cool, dry spot. A locked box if you have kids or pets. A reminder to check expiration dates every six months. And the discipline to throw out what’s old, even if it still looks fine. The posts below cover real stories: how heat ruined a diabetes patient’s insulin, why storing antibiotics in the bathroom led to treatment failure, how one person’s migraine meds turned into dust because of humidity, and what to do when your pharmacy gives you a new bottle that looks nothing like the last one. This isn’t theory. It’s what happens when people don’t know how to store their meds—and what happens when they do.
How to Create a Medication Expiration Review Schedule
Learn how to create a simple, effective medication expiration review schedule to avoid unsafe or ineffective drugs. Know which meds to replace, how to store them, and when to check expiration dates for safety.




