Pancreatitis Warning Signs: Spot the Early Clues
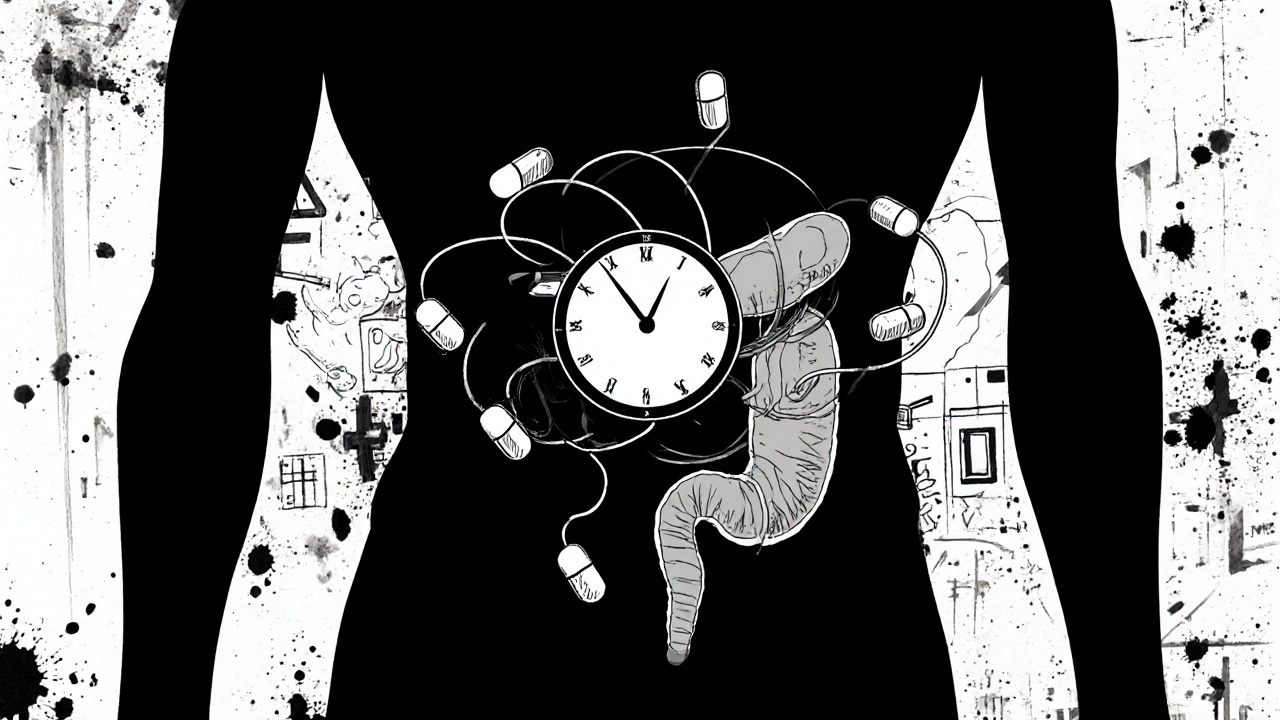
When you hear pancreatitis warning signs, the early symptoms that suggest inflammation of the pancreas. Also known as pancreatitis symptoms, they help patients and clinicians catch the condition before it turns severe.
Understanding these clues starts with the disease itself. Pancreatitis, an inflammation of the pancreas that can be acute or chronic often shows up as a mix of discomfort and systemic signs. One of the most common signals is Abdominal pain, a deep, persistent ache that radiates to the back. This pain isn’t just a tummy ache; it’s usually sharp, worsens after meals, and doesn’t improve with typical over‑the‑counter meds. Another red flag is elevated serum amylase, a blood enzyme that spikes when the pancreas is irritated. When labs show high amylase together with the pain, the odds that you’re dealing with pancreatitis rise dramatically.
Why Spotting Early Signs Matters
Early detection can prevent complications like necrosis, infection, or organ failure. If you notice a sudden onset of nausea and vomiting that doesn’t go away, it’s a signal that the pancreas may be struggling. Jaundice—yellowing of the skin and eyes—can appear when gallstones block the bile duct, a common trigger for pancreatitis. These warning signs often appear together, forming a pattern that clinicians use to decide on imaging tests such as a CT scan or abdominal ultrasound. In practice, pancreatitis warning signs guide the decision to admit a patient, start IV fluids, and monitor for worsening inflammation.
Risk factors also shape the symptom picture. Heavy alcohol use, gallstones, and very high triglyceride levels each raise the chance of developing pancreatitis. People with these backgrounds should be extra vigilant about any new abdominal discomfort or unexplained nausea. Even mild, intermittent pain that’s dismissed as heartburn can be an early warning sign, especially if it’s linked to meals high in fat. Paying attention to the timing, intensity, and accompanying signs—like fever or a rapid pulse—helps differentiate a harmless indigestion from a serious pancreatic event.
When you’re unsure, a quick self‑check can be useful: Do you have sudden, severe upper‑abdominal pain that radiates toward the back? Is the pain worse after eating, especially fatty meals? Are you feeling nauseous, vomiting, or noticing a yellow tint to your skin? Do you have a history of alcohol use, gallstones, or high triglycerides? If you answer yes to several of these, it’s worth contacting a healthcare provider promptly. Early labs can confirm elevated amylase or lipase, and imaging can reveal inflammation or blockage. Acting fast not only eases discomfort but also cuts down on hospital stays and long‑term damage.
All of this ties back to the core idea that pancreatitis warning signs encompass abdominal pain, nausea, jaundice, and lab abnormalities. By recognizing the pattern—pain plus vomiting plus a possible yellow hue—you’re essentially applying a natural diagnostic algorithm that doctors use. This approach empowers you to seek care at the right moment, turning vague discomfort into a clear call for medical evaluation.
Below you’ll find a curated collection of articles diving deeper into each of these signals, the latest testing methods, and practical steps to manage risk factors. Whether you’re looking for how to interpret lab results, what lifestyle changes can lower your risk, or tips on when to call emergency services, the posts ahead cover the full spectrum of information you need to stay ahead of pancreatitis.
Medication‑Induced Severe Pancreatitis: Warning Signs and Treatment
Learn how to spot medication‑induced severe pancreatitis, identify high‑risk drugs, and follow a step‑by‑step treatment plan that can save lives.




