Statins and ALS: What the Research Says About Muscle Drugs and Neurodegeneration
When you take a statin, a class of cholesterol-lowering drugs like atorvastatin or rosuvastatin used to prevent heart attacks and strokes. Also known as HMG-CoA reductase inhibitors, they work by blocking an enzyme your liver needs to make cholesterol. Millions rely on them daily—but questions have surfaced about whether these drugs might play a role in ALS, amyotrophic lateral sclerosis, a progressive nerve disease that causes muscle weakness, loss of movement, and eventually impacts breathing. Also known as Lou Gehrig’s disease, it affects about 5,000 people in the U.S. each year. Some patients and doctors noticed muscle fatigue or cramping after starting statins, and a few studies wondered if this could be more than coincidence.
Here’s the thing: no study has proven statins cause ALS. But a few large population analyses, including one from the Journal of Neurology, Neurosurgery & Psychiatry, found a small uptick in ALS diagnoses among long-term statin users compared to non-users. That doesn’t mean statins triggered it—it could be that people with early, undiagnosed ALS were more likely to have high cholesterol and got prescribed statins first. It’s chicken-and-egg. The FDA reviewed the data in 2015 and found no clear causal link, but they did add a warning to labels about rare reports of muscle damage and weakness. That’s why it matters: if you’re on a statin and start having trouble climbing stairs, lifting your arms, or speaking clearly, don’t ignore it. Talk to your doctor. It could be something simple like low vitamin D or thyroid issues—but ruling out neurological causes early makes a difference.
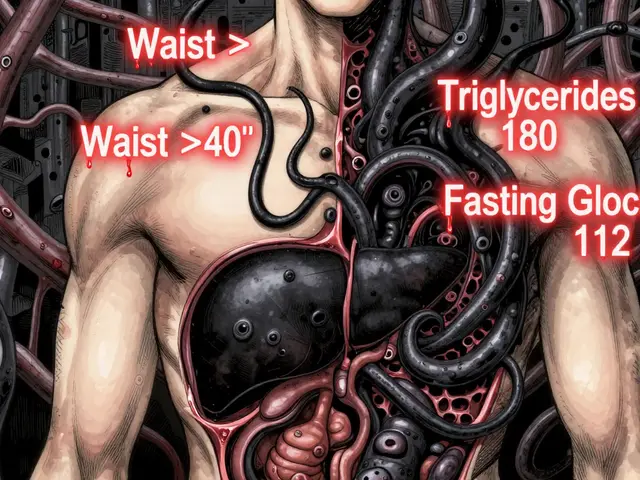
Other related factors show up in the data too. muscle weakness, a common side effect of statins that affects up to 10% of users, often mistaken for aging or inactivity can overlap with early ALS symptoms. That’s why doctors check for creatine kinase levels, EMGs, and nerve conduction studies when symptoms appear. Meanwhile, neurodegenerative diseases, a group of conditions including ALS, Parkinson’s, and Alzheimer’s that involve progressive nerve cell loss don’t have cures yet—but managing risk factors like inflammation, cholesterol, and oxidative stress might help slow things down. Some research even suggests statins could have a protective effect in certain brain conditions, which adds more complexity.
What you’ll find in the posts below isn’t speculation—it’s real-world evidence from patients, doctors, and clinical studies. You’ll see how alternate-day statin dosing helps reduce muscle side effects, how drug interactions can worsen nerve-related symptoms, and what to watch for when switching medications. There’s no magic bullet, but knowing what to ask, what to track, and when to push back on a prescription can change outcomes. This isn’t about fear—it’s about awareness. If you’re on a statin and worried, you’re not alone. Let’s look at what the data actually says.

Statins and ALS: What the Latest Evidence Really Shows
Statins do not cause ALS. Large studies show no link between statin use and ALS risk or progression. In fact, long-term use may reduce ALS risk. Don't stop statins - they protect your heart.