Tricyclic Antidepressants: What They Are, How They Work, and What to Watch For
When you hear tricyclic antidepressants, a class of prescription drugs first developed in the 1950s to treat depression by balancing brain chemicals like serotonin and norepinephrine. Also known as TCAs, they’re not the first choice today—but they’re still used when newer meds don’t work or when patients have chronic pain along with depression. Unlike SSRIs, which target just one chemical, tricyclics hit multiple targets, which is why they can help with nerve pain, migraines, and even sleep issues—but also why they come with more side effects.
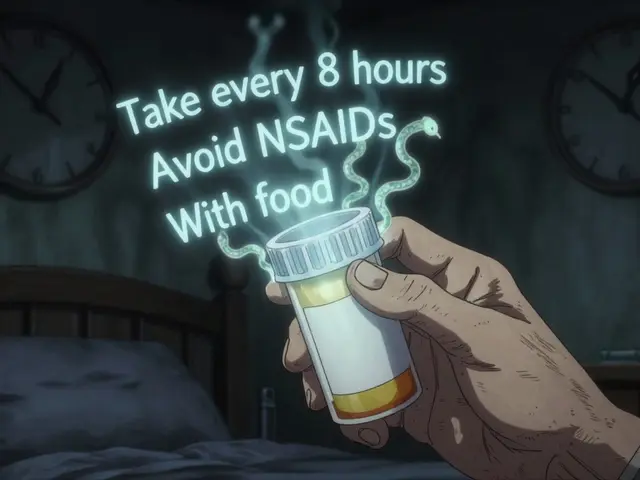
People often stop taking them because of dry mouth, dizziness, weight gain, or feeling foggy in the morning. These aren’t just annoyances—they can make you less likely to stick with the treatment. That’s why medication adherence, how consistently someone takes their prescribed drugs matters so much with TCAs. If you miss doses or quit cold turkey, you risk withdrawal symptoms like nausea, headaches, or even rebound anxiety. And if you’re on other meds—like heart drugs, painkillers, or even herbal supplements like goldenseal, a common herb that interferes with liver enzymes that break down many antidepressants—the risks get even higher. Drug interactions aren’t theoretical; they can land you in the ER.
Some folks stick with tricyclics because they’ve tried everything else. Others use them for conditions like fibromyalgia or nighttime bedwetting in kids. But they’re not for everyone. If you’ve had heart problems, glaucoma, or trouble urinating, your doctor might avoid them entirely. And while newer antidepressants are easier to tolerate, TCAs still work for a surprising number of people who’ve been told they’re "treatment-resistant." The key isn’t just taking them—it’s knowing how to take them safely, recognizing when side effects are normal versus dangerous, and talking to your provider before making any changes.
Below, you’ll find real-world guides on managing side effects, staying on track with meds, spotting dangerous interactions, and understanding why some people switch—or stick—with older drugs like these. These aren’t theory pieces. They’re from people who’ve lived with these meds, and the advice is practical, no-fluff, and straight from experience.

Tricyclic Antidepressant Side Effects: Amitriptyline, Nortriptyline, and Other TCAs Explained
Tricyclic antidepressants like amitriptyline and nortriptyline are still used for depression and nerve pain, but they come with serious side effects including dry mouth, heart risks, and cognitive decline. Learn what you need to know before taking them.