Medication Side Effect Timeline Calculator
This calculator shows typical time-to-onset patterns for common medication side effects based on drug class. Note that individual reactions may vary significantly.
Ever started a new medication and felt something off-muscle pain, dizziness, swelling-but weren’t sure if it was the drug or just bad luck? You’re not alone. Many people assume side effects show up right away, but that’s not always true. Some hit within hours. Others creep in after weeks or even months. Knowing when side effects typically appear for different drugs can save you from misdiagnosis, unnecessary tests, or even stopping a medicine you actually need.
Why Timing Matters More Than You Think
It’s easy to blame a new pill for any weird feeling that pops up after you start taking it. But your body doesn’t work like a light switch. Some reactions are fast. Others are slow burns. The key is understanding the pattern, not just the timing. Take statins, for example. Most people think muscle aches start right after the first dose. But studies show they often appear between one and four weeks. And here’s the twist: in a major 2021 trial, patients who stopped statins because of muscle pain felt better just as fast when they switched to a sugar pill. That’s the nocebo effect-your brain expecting harm, so it creates the symptoms. Timing alone doesn’t prove causation. But when you combine timing with other clues, you start seeing real signals. This is where time-to-onset (TTO) analysis comes in. It’s not fancy jargon. It’s just tracking how long it takes for a side effect to show up after you start a drug. And it’s now a core part of how regulators and doctors understand safety. The World Health Organization and the FDA use it to spot hidden risks. Companies building new drugs have to prove they understand these patterns before approval.Fast-Onset Reactions: Hours to Days
Some side effects are like a lightning strike. They happen fast-and you know it. Angioedema from ACE inhibitors (like lisinopril or enalapril) is a classic. If it’s caused by histamine, swelling in your lips, tongue, or throat shows up within minutes to hours. But if it’s bradykinin-mediated-the more dangerous kind-it can wait. One patient might get it on day two. Another might not notice it until month four. That’s why doctors now warn: if you’ve been on an ACE inhibitor for months and suddenly develop swelling, don’t dismiss it. It could still be the drug. Antibiotics like ciprofloxacin are another example. Peripheral nerve pain-a tingling, burning feeling in your hands or feet-hits fast. Research from 2025 shows the median time is just two days. And women report it faster than men. That’s not a fluke. It’s a pattern. If you start ciprofloxacin and feel odd sensations in your limbs by day three, it’s worth mentioning to your doctor. Don’t wait for it to get worse. Even acetaminophen (Tylenol) follows a sharp timeline. In overdose cases, liver damage can show up within 24 hours. That’s why emergency rooms look at timing when someone comes in after taking too many pills. If it’s been more than 72 hours, the window for the antidote (NAC) closes. Timing saves lives.Mid-Term Reactions: Days to Weeks
This is where most people get confused. Symptoms show up after you’ve been taking the drug for a while, so you assume it’s something else-stress, aging, a virus. Antiepileptic drugs like pregabalin and gabapentin are common culprits. People take them for nerve pain or anxiety. Side effects like dizziness, fatigue, or brain fog? They show up in the first week for over half of users. But the median time? Nineteen days for pregabalin. Thirty-one for gabapentin. That means if you started two weeks ago and suddenly feel like you’re moving through molasses, it’s probably the medication-not your busy schedule. Statins fall here too. While some people feel muscle pain immediately, most report it after 1-4 weeks. And again, studies show it’s not always the drug. In one trial, 55% of people who stopped statins for muscle pain improved within three days-even if they were given a placebo. But that doesn’t mean it’s all in your head. For some, the drug really is the trigger. The key is recognizing the pattern: if the pain started after two weeks of steady use, and got worse with dose increases, that’s a red flag. Drug-induced hepatitis is another mid-term player. Most cases show up around 42 days after starting the drug. But the range? 20 to 117 days. That’s almost four months. If you’re on antibiotics, antifungals, or even herbal supplements like kava or green tea extract, and you start feeling nauseous, yellow-eyed, or unusually tired after six weeks, get your liver checked. Don’t wait for it to get worse.
Long-Term Reactions: Months to Years
This is the scary part. Some side effects don’t show up until you’ve been on the drug for half a year-or longer. Natalizumab, used for multiple sclerosis, can cause a rare but deadly brain infection called PML. The median time to onset? Over 140 days. Some patients don’t show symptoms until after 18 months. That’s why doctors monitor patients closely every three months with MRI scans. If you’ve been on this drug for a year and suddenly have trouble walking or speaking, don’t think it’s your MS flaring. It could be PML. Timing is everything. Interferon beta-1a, used for MS too, has an even longer tail. One study found the median time to develop peripheral nerve pain was 526.5 days-almost 18 months. That’s longer than most people stay on the drug. If you’ve been taking it for a year and start feeling numbness in your feet, your doctor might not connect it. But research says: it’s possible. Even common drugs like metformin can have delayed reactions. Lactic acidosis is rare, but when it happens, it’s often after months of use, especially if kidney function slowly declines. That’s why annual kidney tests are recommended.What Makes Timing Different Between Drugs?
Why do some drugs act fast and others take forever? It comes down to how they work in your body. Drugs that directly irritate tissue-like ciprofloxacin damaging nerves-hit fast. Their chemistry is aggressive. Others, like immune-modulating drugs, work by slowly changing your body’s defenses. That takes time. Natalizumab blocks immune cells from entering the brain. It doesn’t cause damage right away. It lets a dormant virus wake up over months. Your genetics matter too. Some people metabolize drugs slowly. That means the drug builds up over time. Others have enzymes that break it down fast. That’s why two people on the same dose can have totally different timing for side effects. Sex also plays a role. Women are more likely to experience certain side effects earlier. For ciprofloxacin, women get nerve pain at two days. Men? Four days. That’s not a small difference. It’s a pattern.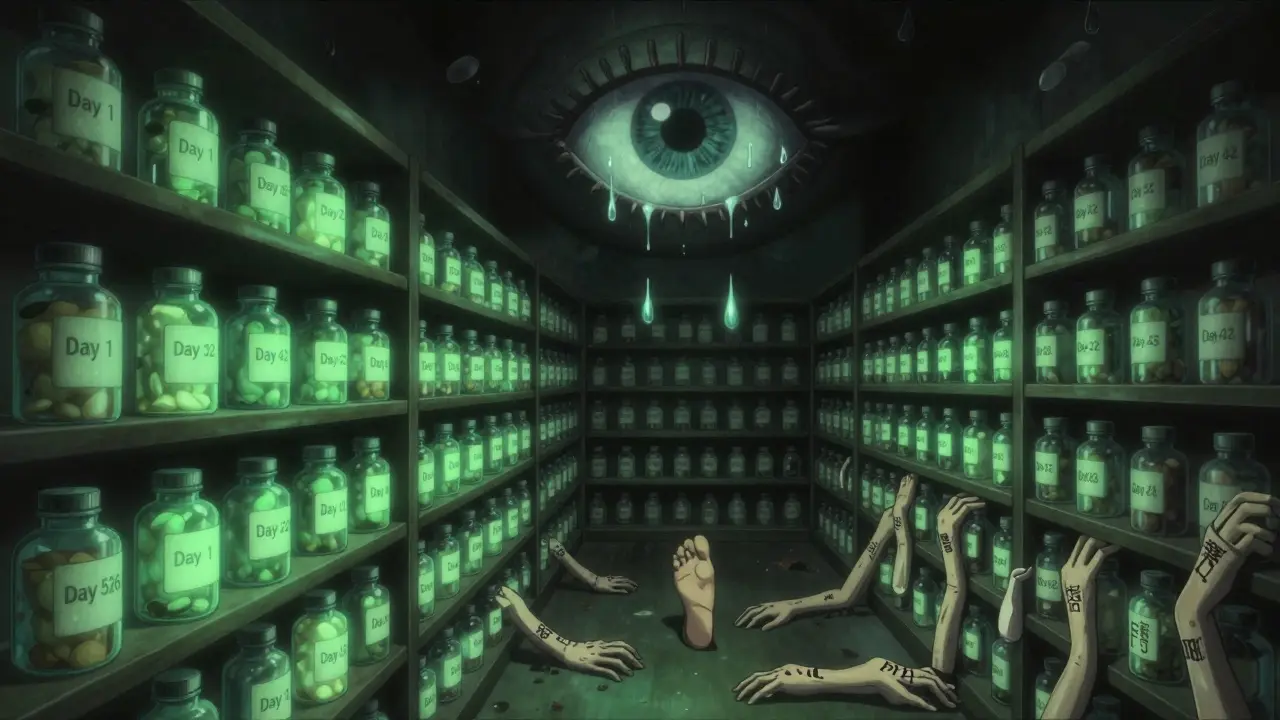
How Doctors Use This Info
Hospitals aren’t just guessing anymore. Electronic health records now have built-in tools that flag side effects based on timing. Mayo Clinic’s system started catching 22% more reactions after adding TTO logic. If you start a new drug and get diarrhea on day 12, the system might pop up: “Possible Clostridioides difficile infection. Common onset: 5-10 days.” That’s not magic. It’s data. The FDA requires drug makers to report TTO patterns. The European Medicines Agency has made Weibull distribution analysis mandatory since 2020. That’s a statistical model that predicts whether risk increases, decreases, or stays steady over time. It’s how they know if a side effect is early, late, or random. And it’s changing labeling. More drug inserts now say: “Side effects may appear after several weeks.” That’s new. Ten years ago, most just said “may occur.” Now, they’re getting specific.What You Should Do
You don’t need to be a scientist. But you can use this info to be smarter.- When you start a new drug, ask: “What’s the most common time frame for side effects?”
- Write down when you started and when symptoms began. Don’t rely on memory.
- If you get a side effect after six months, don’t assume it’s unrelated. Check the research.
- Don’t panic if a side effect shows up early. It might be temporary. But don’t ignore it either.
- Track whether symptoms improve after stopping the drug. If they do within a few days, that’s a strong clue.






9 Comments
Darren Gormley
January 31, 2026 AT 05:37 AMLmao so now we're treating drug side effects like a fucking weather forecast? 🤡 Next they'll tell us when to expect a 'statin thunderstorm' at 3pm on Tuesday. I've been on lisinopril for 8 months and my lips swell every time I eat sushi. Coincidence? Or just my body being dramatic?
Claire Wiltshire
February 2, 2026 AT 04:39 AMThis is an excellent, clinically nuanced overview. Many patients (and even some providers) overlook the temporal relationship between medication initiation and symptom onset. The nocebo effect is profoundly underappreciated in clinical practice. Tracking time-to-onset isn't just useful-it's essential for evidence-based de-escalation. I've personally seen patients discontinue effective statins due to misattributed myalgia, only to realize their symptoms resolved with placebo. Timing, context, and exclusion criteria matter more than we assume.
Russ Kelemen
February 2, 2026 AT 15:29 PMI love how this post frames side effects as a conversation-not a punishment. Your body isn't fighting the drug, it's trying to understand it. That shift in perspective changes everything. I used to panic when I felt weird after a new med. Now I ask: 'What's the rhythm here?' Sometimes it's the drug. Sometimes it's stress. Sometimes it's just your nervous system catching up. The key isn't to fear the signal-it's to learn its language.
Adarsh Uttral
February 3, 2026 AT 13:42 PMbro i started metformin 3 months ago and my legs felt like jelly last week. i thought it was my new gym routine. turns out its the drug? wow. i just stopped taking it and feel better already. thanks for the heads up lol
Diksha Srivastava
February 3, 2026 AT 20:19 PMThis is so empowering!! I used to think if I felt weird after a week, I was just being dramatic. Now I know my body’s not broken-it’s just talking! 🙌 Keep sharing this kind of info, it helps people feel less alone in their health journey!
owori patrick
February 5, 2026 AT 01:49 AMI'm from Nigeria and we don't always have access to fancy tracking tools, but I've seen this firsthand. My aunt took an antifungal for a foot rash and got liver issues after 10 weeks. Doctors thought it was hepatitis B. Turned out it was the drug. We need this knowledge everywhere-not just in the US or UK.
April Allen
February 5, 2026 AT 14:02 PMThe Weibull distribution modeling referenced here is a critical advancement in pharmacovigilance. The hazard function’s shape-whether increasing, decreasing, or constant-provides probabilistic insight into the underlying biological kinetics. This moves us beyond binary 'drug-caused' assumptions into dynamic risk stratification. The NIH’s All of Us initiative will likely integrate this with pharmacogenomic biomarkers (e.g., CYP2D6, SLCO1B1) to generate individualized TTO probability curves. Expect FDA labeling to evolve accordingly within 24 months.
Sidhanth SY
February 6, 2026 AT 15:38 PMHonestly, I didn't think about timing until I got nerve pain from cipro after 3 days. My doctor said it was 'probably anxiety.' I didn't believe him. Went back two weeks later with a symptom log. He apologized. Point is: write it down. Even if it seems small.
Mike Rose
February 7, 2026 AT 12:53 PMso like... if i feel weird after taking a pill, it might be the pill? wild. i thought it was just me being a hypochondriac lol