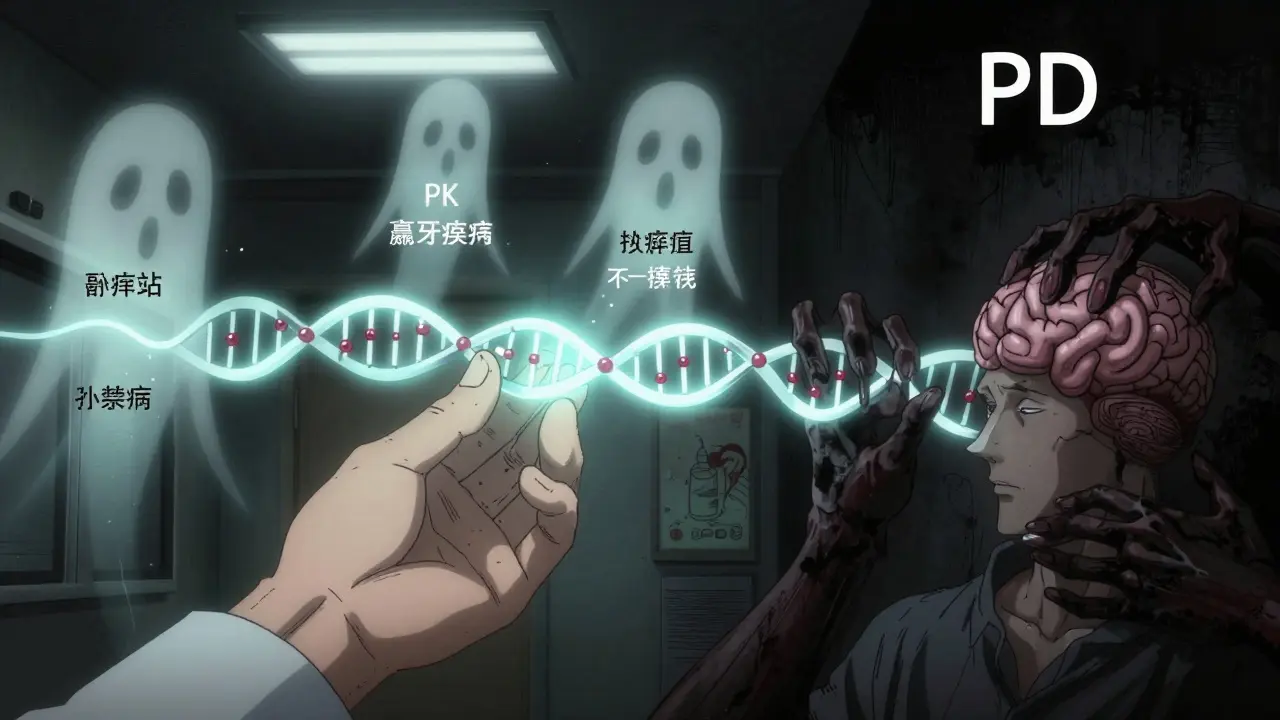
PK/PD Drug Interaction Quiz
Test Your Knowledge
Take this 5-question quiz to see how well you understand pharmacokinetic (PK) vs pharmacodynamic (PD) drug interactions. Answer each question, then check your score at the end.
When you take more than one medication, something unexpected can happen-even if each drug works fine on its own. Two drugs might clash in ways you can't see, leading to dangerous side effects or making one of them useless. This isn't rare. About 15% of adults over 65 take five or more medications daily, and nearly half of all serious drug interactions happen because of how these drugs interact inside your body. The key to avoiding harm? Understanding the difference between pharmacokinetic and pharmacodynamic interactions.
What Pharmacokinetic Interactions Really Mean
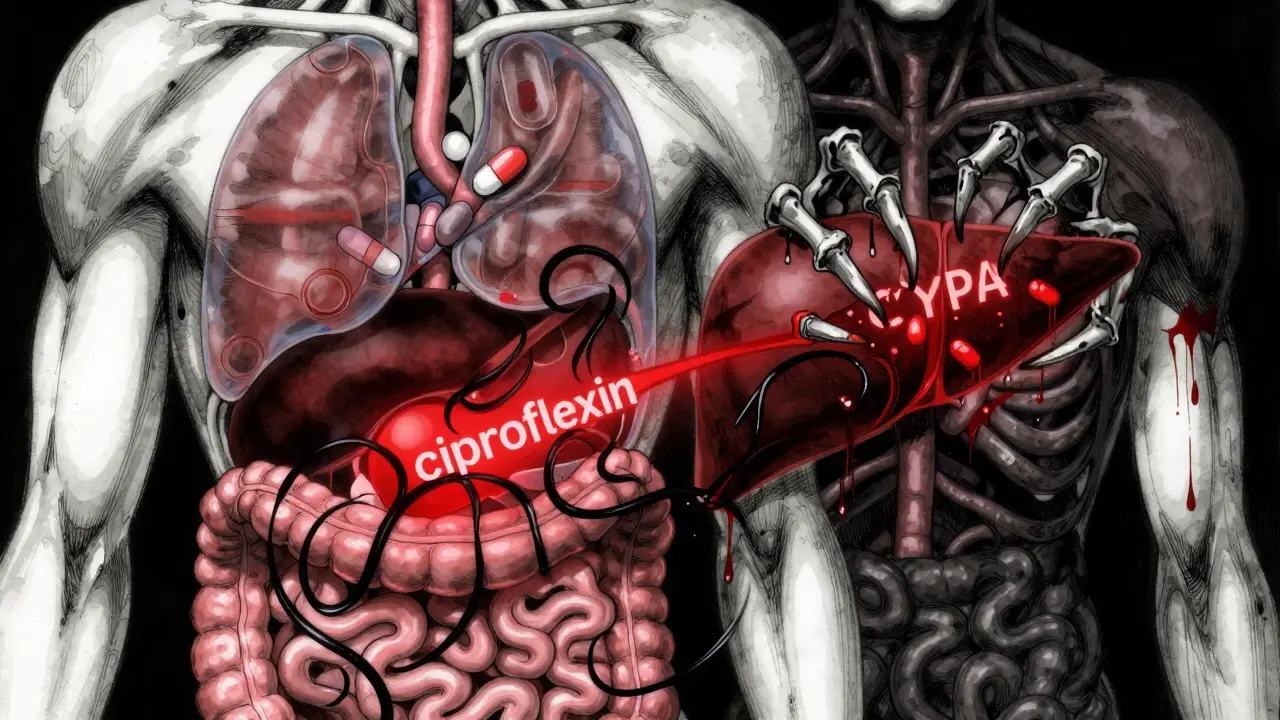
Pharmacokinetic, or PK, interactions are about what your body does to the drug. Think of it like a delivery system. Your body absorbs, distributes, metabolizes, and gets rid of drugs. If one drug messes with any of those steps, it changes how much of the other drug reaches its target. That’s where problems start.Take ciprofloxacin, an antibiotic. If you take it with an antacid like Tums, the magnesium or aluminum in the antacid binds to the antibiotic in your gut. This cuts its absorption by 75-90%. You might think you’re getting the full dose, but your body never sees enough of it. The infection doesn’t clear, and you might end up back at the doctor.
Another big player is liver metabolism. About 75% of all drug interactions happen because of enzymes in the liver-especially CYP3A4, CYP2D6, and CYP2C9. These enzymes break down drugs so your body can flush them out. But some drugs block or speed up these enzymes. For example, clarithromycin (an antibiotic) shuts down CYP3A4. When that happens, simvastatin (a cholesterol drug) builds up in your blood by 10 times. That can cause muscle damage, kidney failure, or even death. The FDA recommends cutting simvastatin to 10 mg or avoiding it entirely if you’re on clarithromycin.
Then there’s protein binding. Drugs like warfarin stick to proteins in your blood so they don’t act too fast. But if another drug, like phenylbutazone, kicks warfarin off those proteins, suddenly you’ve got three times more active warfarin floating around. That’s a recipe for internal bleeding. This is why your INR levels get checked often if you’re on warfarin and start a new med.
Excretion matters too. Probenecid, used for gout, blocks the kidney’s ability to clear penicillin. That’s actually intentional-it’s used to boost penicillin levels in infections like syphilis. But if you’re not aware of it, you might think the penicillin isn’t working because you’re not seeing improvement-when really, it’s working too well.
What Pharmacodynamic Interactions Really Mean
Pharmacodynamic, or PD, interactions are about what the drug does to your body. It doesn’t matter how much drug is in your blood. If two drugs hit the same system, they can amplify, cancel, or distort each other’s effects.Think of it like a seesaw. One drug pushes down, another pushes up. Or both push down together. That’s what PD interactions look like.
One of the scariest examples is sildenafil (Viagra) and nitrates (used for chest pain). Both relax blood vessels. Together, they can drop your blood pressure so hard you go into shock. This combo is absolutely contraindicated. No dose adjustment helps-just don’t mix them.
Another common one is SSRIs (antidepressants) and MAO inhibitors. Both increase serotonin. Together, they can trigger serotonin syndrome: high fever, seizures, rigid muscles, and confusion. It’s life-threatening. Doctors won’t even prescribe them within weeks of each other.
But not all PD interactions are obvious. Take NSAIDs like ibuprofen and ACE inhibitors like lisinopril. The ACE inhibitor lowers blood pressure by blocking a hormone. The NSAID blocks prostaglandins, which help keep blood vessels open. Together, the ACE inhibitor loses about 25-30% of its effect. Your blood pressure stays high, and you don’t even know why.
And then there’s additive effects. Warfarin and aspirin both thin the blood. Alone, each is safe. Together? Your risk of bleeding jumps dramatically. You might not realize it until you bruise easily or notice blood in your stool.
The Key Difference: Concentration vs. Response
Here’s the simplest way to tell them apart:- PK interactions change the amount of drug in your system.
- PD interactions change how your body responds to that drug.
That difference changes everything in how you manage them.
With PK interactions, you can often fix things by adjusting the dose or timing. If a drug is being broken down too fast, you increase the dose. If it’s building up, you lower it. Therapeutic drug monitoring (TDM) helps here-measuring blood levels of drugs like digoxin or phenytoin to stay in the safe zone.
But PD interactions? You can’t dose your way out of them. If two drugs both depress your breathing, no amount of tweaking will make it safe. You have to avoid the combo entirely. That’s why the FDA and EMA list so many contraindications-not because the drugs are bad, but because their effects stack dangerously.
Dr. David E. Golan put it best: “PK interactions shift the dose-response curve sideways. PD interactions shift it up or down.” In plain terms: PK changes how much drug you need. PD changes how the drug works, no matter the dose.

Which Type Is More Dangerous?
It’s not about which is worse-it’s about which is harder to catch.PK interactions are more common with drugs that have a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. Warfarin, digoxin, and lithium fall here. About 68% of serious interactions with these drugs are PK-based. That’s why your blood levels get checked regularly.
But PD interactions are sneakier. They don’t show up on lab tests. You can have perfect drug levels and still overdose on effects. That’s why 85% of CNS drug interactions-like those involving opioids, benzodiazepines, and antipsychotics-are PD-based. A patient might be on three drugs that all make them sleepy. Their blood levels look fine. But they’re nodding off in the middle of the day. No one connects the dots until they fall.
And here’s the scary part: PD interactions are often overlooked. A 2023 study found that 70% of adverse events from PD interactions weren’t flagged by electronic systems because they didn’t involve enzyme changes. They were just “both drugs make you tired.” That’s not enough to trigger an alert.
How Clinicians Manage These Interactions Today
Electronic health records now flag thousands of interactions. Epic’s 2023 update alone warns about 1,247 high-severity PK interactions and 983 high-severity PD interactions. But alerts can be overwhelming. Pharmacists are the real gatekeepers.Pharmacist-led medication reviews cut adverse events by 42%. How? They don’t just look at the list of drugs. They ask:
- Is this a PK interaction? Then check levels. Adjust dose. Delay one drug.
- Is this a PD interaction? Then ask: Can we swap one drug? Can we space them out? Or do we need to stop one completely?
For example, if someone is on fluoxetine (an SSRI) and needs an antibiotic, the pharmacist won’t pick clarithromycin. Even though it’s effective, it’s a CYP2D6 inhibitor-and fluoxetine is metabolized by that enzyme. The combo could raise fluoxetine levels dangerously. Instead, they choose azithromycin, which doesn’t interfere.
For PD risks, they use clear monitoring rules:
- For CNS depressants: respiratory rate below 12 breaths/min? Oxygen below 90%? Stop the combo.
- For anticoagulants: INR over 4.0? Time to reassess.
- For blood pressure drugs: systolic drop over 30 mmHg? You’ve got a PD interaction.
The Future: AI, Genes, and Real-World Data
The tools are getting smarter. The FDA now requires testing interactions with 11 CYP enzymes and 8 transporters-up from 7 in 2017. That means new drugs are being vetted more thoroughly.Pharmacogenomics is changing the game too. If you’re a poor metabolizer of CYP2D6 (about 7% of people), even a normal dose of certain drugs can be toxic. CPIC now has 32 gene-drug pairs with clear guidelines. Your DNA can tell you if you’re at risk before you even take the pill.
Real-world data from the FDA’s Sentinel Initiative found 17 new PD interactions in 2022. One example: SGLT2 inhibitors (like dapagliflozin) plus loop diuretics (like furosemide) increase dehydration risk by 2.3 times. That’s not something you’d predict from lab studies alone.
And AI? A 2023 model in Nature Medicine predicted PD interactions with 89% accuracy. Traditional methods? Only 76%. That’s a big leap. In five years, your doctor’s system might warn you not just about drug combos, but about your personal risk based on age, kidney function, genetics, and even your diet.
What You Should Do
If you’re on multiple medications:- Always tell your doctor and pharmacist about every drug-including vitamins, herbs, and OTC painkillers.
- Ask: “Could this interact with anything else I’m taking?” Don’t assume it’s safe.
- If you start a new drug and feel weird-dizzy, nauseous, overly sleepy-don’t ignore it. Call your pharmacist. It might be a PD interaction.
- Get your blood tested if you’re on warfarin, digoxin, or lithium. Levels matter.
- Don’t skip doses just because you’re worried. Talk to someone first. Stopping suddenly can be just as dangerous.
Drug interactions aren’t about bad drugs. They’re about complex biology. The more you know, the safer you are.
What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic (PK) interactions change how your body processes a drug-like how fast it’s absorbed, broken down, or cleared. Pharmacodynamic (PD) interactions change how the drug affects your body, even if the drug level stays the same. PK is about concentration; PD is about effect.
Can pharmacokinetic interactions be fixed with dose changes?
Yes, often. If a drug builds up because another drug blocks its metabolism, lowering the dose can help. Therapeutic drug monitoring (measuring blood levels) is commonly used for drugs like warfarin or digoxin to guide these adjustments.
Why are pharmacodynamic interactions harder to predict?
Because they don’t show up in blood tests. Two drugs might have perfect levels but still cause dangerous side effects when combined-like excessive drowsiness or low blood pressure. You can’t measure a response the way you measure a concentration.
Which drugs are most likely to cause serious interactions?
Drugs with a narrow therapeutic index-like warfarin, digoxin, lithium, and phenytoin-are high-risk for PK interactions. For PD interactions, CNS drugs (opioids, benzodiazepines, SSRIs), antihypertensives, and anticoagulants are most common. Combining any of these with other similar drugs increases danger.
Do herbal supplements cause these interactions?
Absolutely. St. John’s Wort speeds up metabolism of many drugs (PK), making birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can thin the blood (PD), raising bleeding risk with warfarin or aspirin. Always tell your provider about supplements-they’re not harmless.
How can I check for interactions before taking a new drug?
Ask your pharmacist. They have access to updated databases that screen for over 2,000 interactions. You can also use trusted apps like Micromedex or Lexicomp, but never rely on generic internet searches. Your pharmacy’s system is updated daily with new clinical evidence.
Next Steps
If you’re managing multiple medications:- Keep a written list of everything you take-name, dose, reason, and time.
- Bring it to every appointment, even if you think nothing changed.
- If you’re over 65 or have kidney/liver disease, ask if your drugs need special monitoring.
- Don’t wait for side effects. Prevention beats reaction.
Understanding PK vs PD isn’t just for doctors. It’s your safety net.


1 Comments
Shalini Gautam
February 21, 2026 AT 18:45 PMAs an Indian woman who’s seen her grandma juggle 7 pills a day, I’m so glad this breakdown exists. PK vs PD isn’t just jargon-it’s life or death. My aunt took warfarin and turmeric supplements thinking ‘natural = safe.’ Turns out, turmeric’s a PD nightmare-thins blood like aspirin. She ended up in the ER. Now she carries a printed list. Everyone should.
PS: If you’re on meds, don’t trust Google. Talk to your pharmacist. They’re the real superheroes.