H2 Blockers: What They Are, How They Work, and What You Need to Know
When your stomach makes too much acid, it can cause heartburn, ulcers, or GERD. That’s where H2 blockers, a class of medications that reduce stomach acid by blocking histamine receptors in the stomach lining. Also known as histamine blockers, they work by telling acid-producing cells to calm down—no magic, just chemistry. Unlike antacids that just coat the stomach, H2 blockers go straight to the source and turn down the acid faucet. They’re not new—some have been around since the 1970s—but they’re still a go-to for millions who need fast, reliable relief without popping pills every hour.
There are a few common types you might recognize: ranitidine (Zantac), famotidine (Pepcid), cimetidine (Tagamet), and nizatidine (Axid). But not all are still on the market. Ranitidine got pulled in many countries after concerns about a possible cancer-causing contaminant. That left famotidine as the most widely used today, available both by prescription and over the counter. These drugs don’t cure the root cause of acid problems, but they give your stomach lining time to heal. That’s why doctors often pair them with lifestyle changes—like avoiding spicy food, eating earlier, or cutting back on alcohol.
What’s interesting is how H2 blockers fit into the bigger picture of stomach health. They’re often compared to PPIs (proton pump inhibitors), which block acid more completely. But PPIs come with more long-term risks—like nutrient deficiencies or bone loss. H2 blockers? Safer for occasional use. They’re also less likely to interfere with other meds, which matters if you’re on blood pressure pills, antibiotics, or antidepressants. And unlike PPIs, they work fast—often within an hour. That’s why some people keep a bottle of Pepcid in their drawer for late-night heartburn or after a big meal.
But they’re not for everyone. If you have kidney problems, your body can’t clear these drugs as easily. Older adults may feel dizzy or confused after taking them. And while they’re generally safe for short-term use, long-term use without medical supervision can hide something more serious—like a stomach ulcer or even cancer. That’s why it’s smart to talk to your doctor if you’re using them more than twice a week for over a month.
What you’ll find in the posts below isn’t just a list of H2 blockers. It’s real-world guidance on how these drugs interact with other meds, how they affect your body over time, and what to watch for when switching treatments. You’ll see how acid control ties into broader issues like medication adherence, drug interactions, and even how your liver processes these compounds. Whether you’re managing heartburn, dealing with a prescription change, or just trying to understand why your pill looks different now, these posts give you the facts without the fluff.
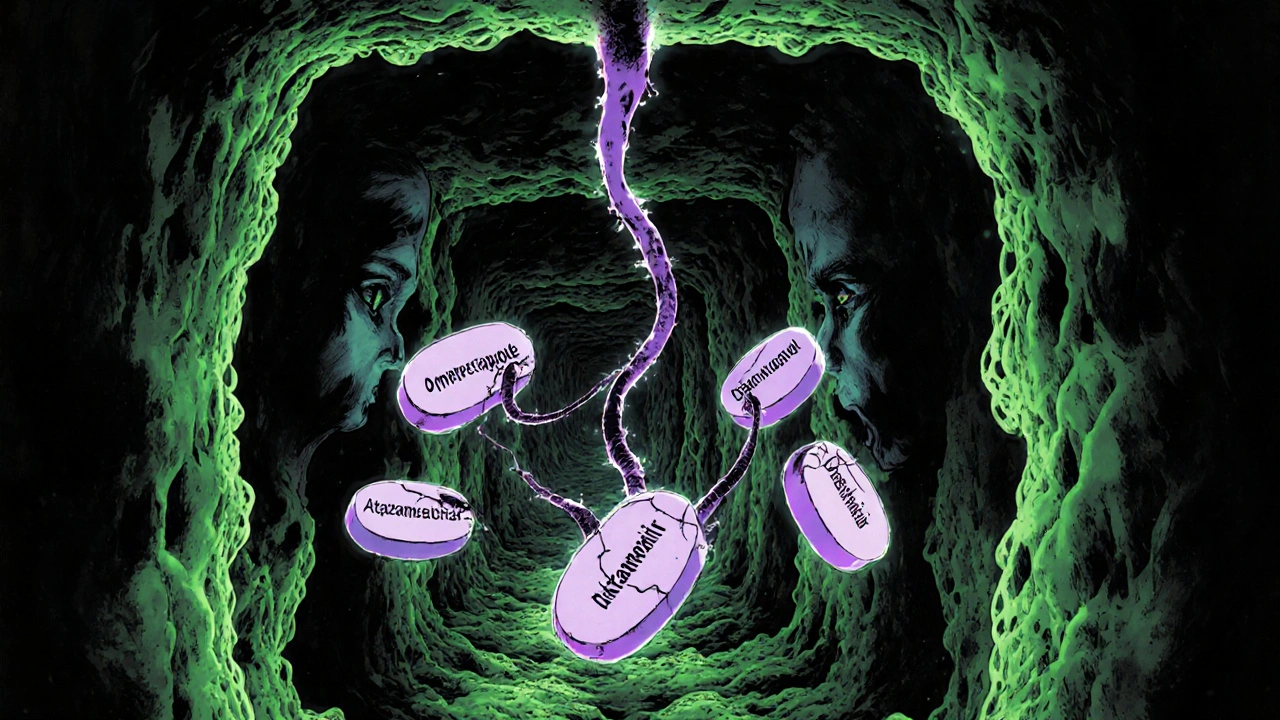
Acid-Reducing Medications: How They Interfere With Other Drugs
Acid-reducing medications like PPIs can severely reduce absorption of critical drugs like HIV treatments and cancer therapies. Learn which medications are at risk and how to protect your treatment.